Introduction
Governments across the globe implement powerful measures and allocate adequate resources to support their respective healthcare systems. The involvement of different stakeholders, professionals, and partners remains critical to ensure that timely results are recorded. The Spanish healthcare model remains one of the best in Europe and across the globe. The relevant institutions and policymakers consider the best models, solve emerging challenges, and consider evidence-based approaches to improve the nature of care delivery. This thesis paper describes and critiques the Spanish health system and proposes appropriate strategies to address possible shortcomings that might emerge in the near future.
Context
Spain is one of the economically and politically progressive nations in the European Union (EU). Just like the other nations, histories of monarchs and immigrants have continued to dictate experiences and cultural relations in Spain. By 2018, the World Health Organization (WHO) identified Spain as a country whose life expectancy was above 82 years (Bernal-Delgado et al. 2018). However, the country’s elderly population is higher in comparison with people below 60 years of age.
Population growth rate in Spain has remained significantly low within the past three decades. Specifically, the country’s has a population of around 48 million citizens and a physical size of 505 thousand square kilometers. From the beginning of the 21st century, the country recorded an increasing number of immigrants, thereby transforming economic, demographic, and social dynamics.
The healthcare sector has been expected to remain resilient and continue focusing on the best ways to meet the demands of all citizens. However, some trends and challenges exist that affect the nature of the anticipated goals. For instance, respiratory infections, cancer, and cardiovascular diseases form the primary causes of premature deaths in Spain (Avanzas, Isaac and Moris 2017). Constants improvements have been recorded in a number of key areas, including maternal health, smoking reduction, and diet management. However, unique predicaments continue to affect the medical experiences and outcomes of more people negatively, such as overweight, obesity, alcohol consumption, and smoking. Fortunately, the government has been keen to consider and implement evidence-based measures and strategies to improve the situation and meet the demands of more citizens or underserved populations.
Healthcare System
The passage of Spain’s General Healthcare Act of 1986 gave room for developing the Spanish National Healthcare System. Currently, the framework is designed in such a way that all citizens have access to universal medical coverage. This arrangement does not consider people’s economic positions or enrolment in the country’s social security program. To support the effectiveness of the system, the government has promoted three organizational levels that meet the demands of the targeted beneficiaries.
First, the Central Administration comprises of the Ministry of Health (MoH) as the leading administrator or agency. The involved leaders in the MoH will provide ideas, implement guidelines, and plan for activities. Second, Autonomous Communities are developed and designed in such a way that they provide the relevant medical services at the regional level (Avanzas, Isaac and Moris 2017). Third, Local Agencies, also called Areas de Salud, are designed to focus n climatic patterns, demographics, employment situations, cultural attributes, and socioeconomic aspects. Those involved in the third level will consider the best ways to maximize efficiency and divide regions to ensure that more people get timely medical services.
To streamline operations, the country promotes these two unique systems: private and public. The public one is designed in such a way that it meets the medical demands of individuals who contribute to the designed social security program. Family members of such citizens would be covered under the public system. Those who are living in poor economic situations and retirees will receive free medical services (Bernal-Delgado et al. 2018). The private system is responsible for providing insurance coverage, meeting patients’ eye and dental services, and providing timely medical information to beneficiaries. Private pharmacies exist whereby specialists are expected to provide timely treatment for minor diseases.
From these arrangements, it is notable that the country promotes a universal healthcare system given the name Spanish National Health System (SNS). This popular model ensures all the people can get free medical cover. Foreigners working officially in Spain will have access to SNS services (Avanzas, Isaac and Moris 2017). Immigrants without the relevant documents will also receive timely medical services whenever they are in any given emergency room. Medical schools and private institutions collaborate with the public system to maximize the overall outcomes of the citizens.
Key Healthcare Issues
Within the past three decades, the Spanish healthcare system has remained resilient and capable of meeting the medical needs of more citizens. Unfortunately, some challenges continue to exist that affect the overall wellbeing and experiences of more individuals. First, the government has witnessed a surging public debt that has affected the healthcare industry directly (Avanzas, Isaac and Moris 2017). Consequently, most of the medical facilities and ambulatory centers are being privatized or closed at an alarming rate. This problem is linked to reduced medical procedures and poor medical experiences. In most of the cases, emergency services tend to be delayed while at the same time overwhelming the medical practitioners.
Second, the country is yet to fully embrace the power of tele-health initiatives and relationships that resonate with the nature and effectiveness of medical informatics. The consideration of such developments in different countries had led to reduced physician burdens and improved care delivery. Spain appears to be reluctant in adopting most of these systems to improve care delivery. Third, the spending rate for the National Health System in this country has been increasing exponentially (Bernal-Delgado et al. 2018). This means that the level of expenditure remains higher in comparison with the country’s economic performance. This predicament has triggered additional challenges or concerns, including increasing cost for drugs and inefficiency of the overall medical care delivery system.
Fourth, the relevant partners and stakeholders have been taking long to review the nature of portfolios and health services that are available in different channels or levels of care delivery. This gap has complicated the scenario and made it impossible for more people to access or pool resources for specialized treatments (Bernal-Delgado et al. 2018). Fifth, the healthcare system lacks managerial autonomy that is capable of supporting the effectiveness of the medical system and ensuring that all involved institutions can provide better strategies and techniques to improve the nature of medical services available to more patients.
Finally, the ongoing coronavirus disease of 2019 (COVID-19) pandemic has presented additional lessons regarding the loopholes and gaps in the Spanish National Health System. Specifically, the emergence of this pandemic overwhelmed all medical systems across the country and eventually led to the deaths of thousands of elderly citizens (Legido-Quiqley et al. 2020). The observations made included the absence of proper mechanisms for preventing possible outbreaks and responding to specific diseases effectively, failure to meet the demands of underserved populations, and absence of superior strategies to respond to national health calamities. These gaps explain why additional changes and improvements would be essential to improve the effectiveness of the country’s healthcare sector.
Critical Appraisal
The WHO offers a detailed framework that countries can follow when planning to develop an effective and resilient healthcare system. According to the agency, a proper system should be comprised of the relevant actions, people, and institutions whose mission is to restore, promote, or maintain the overall outcomes of the population (Bernal-Delgado et al. 2018). The government needs to be involved to offer the relevant resources, solve emerging issues, and identify the major determinants of the population’s health. The collaboration of all actors and funders is essential to support the introduction of activities that help improve health outcomes.
WHO goes further to indicate that an effective system will integrate other efforts that can improve overall health outcomes. Private practitioners, providers, and institutions remain essential to educate and help maximize people’s medical experiences.
From this analysis, it is agreeable that Spain has an effective health system that integrates the relevant building blocks, including private players and public organizations or levels. Private entities, insurers, and institutions are also involved to influence health policies, engage in continuous learning, and identify key gaps that require constant improvement. These key cogs or attributes remain critical towards supporting the effectiveness of the overall healthcare system (Caballer-Tarazona and Vivas-Consuelo 2016). The government relies on the available policymaking mechanisms to make laws and guidelines for the MoH to implement.
These initiatives have made it possible for the country to have an effective healthcare model. Additionally, the Spanish government relies on taxation to finance the healthcare system (Ródenas and Garcés 2017). The model meets the medical needs of around 99.7 percent of the general population while the private sector provides services to the remaining 0.3 percent (Ródenas and Garcés 2017). Individuals can provide out-of-pockets and co-payments to support private funding.
The effectiveness of the outlined three levels and the involvement of the private sector are attributes that ensures that the system helps implements proper mechanisms to help improve health outcomes. The government is directly at the center to implement policies, monitor the missions of different participants, and solve most of the recorded challenges. Different partner organizations engage in continuous research and development (R&D) to solve some of the recorded issues and present better initiatives to improve the system (Ródenas and Garcés 2017). While some gaps exist, the country has succeeded in meeting the demands of more citizens and foreigners in need of high-quality and personalized medical services.
In terms of responsiveness, it is agreeable that the health system is capable of relying on the presented information about the key determinants of health. Due to the nature of the promoted mechanisms, the system remains responsive since the professionals and leaders are always keen to meet the legitimate demands of all citizens. To do so, all participants are keen to promote a number of elements, such as social support, autonomy, confidentiality, dignity, choice of medical options and providers, and prompt attention (Legido-Quiqley et al. 2020). The popular system continues to meet the medical demands of most of the patients in this country.
Within the Spanish context, proper administrative and clinical procedures and models exist that are intended to identify and mitigate social issues and risks. The relevant agencies monitor key risk factors and social determinants of health in order to respond accordingly. Risk management strategies have led to proactive initiatives and efforts that are intended to safeguard the level of patient safety (Caballer-Tarazona and Vivas-Consuelo 2016). Organizations receive timely guidelines and opportunities for assessing healthcare needs, brand value, and expectations. Collaborative efforts exist that make it possible for system to reduce risks and improve the overall medical experiences of more citizens in the country.
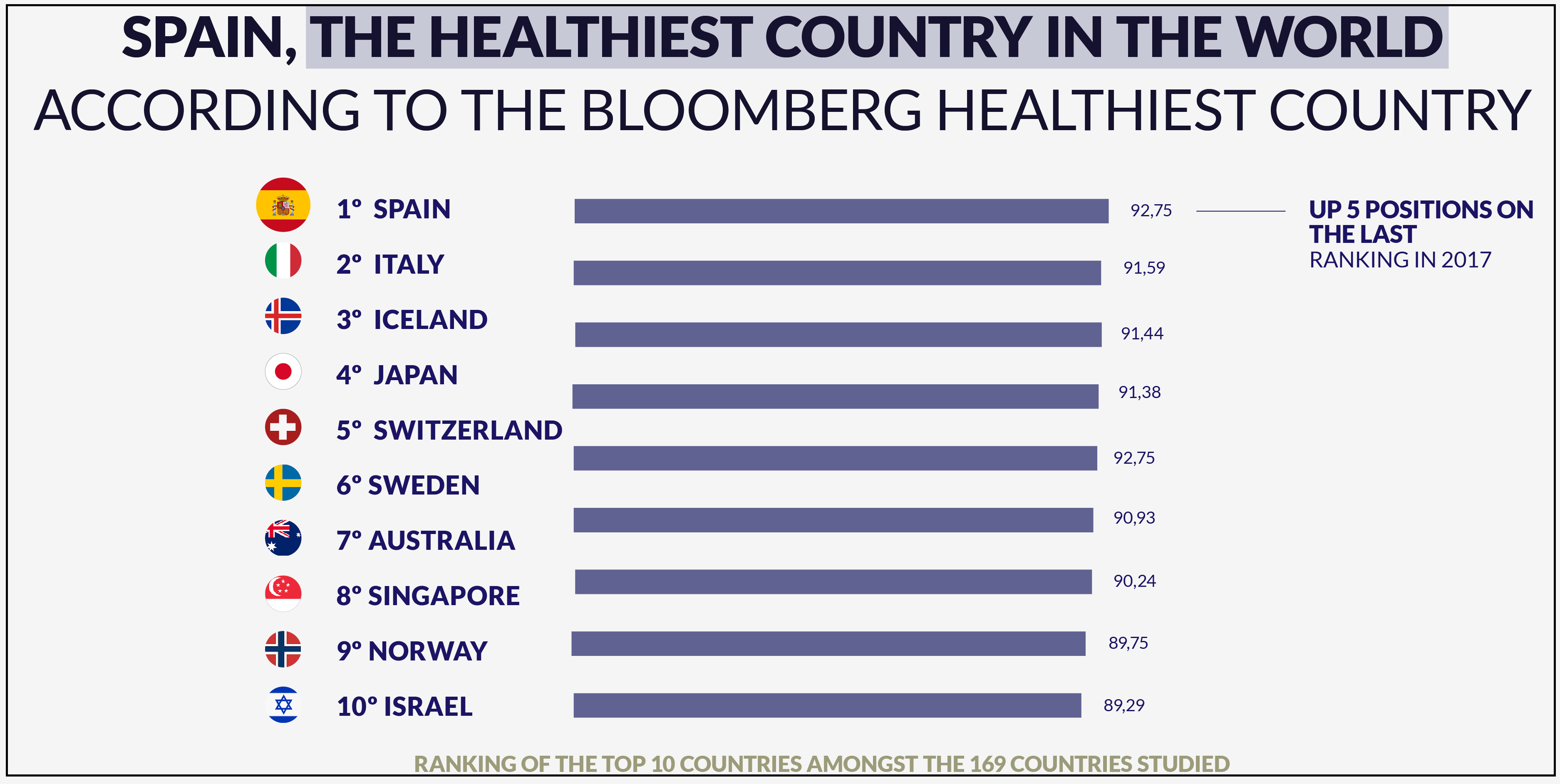
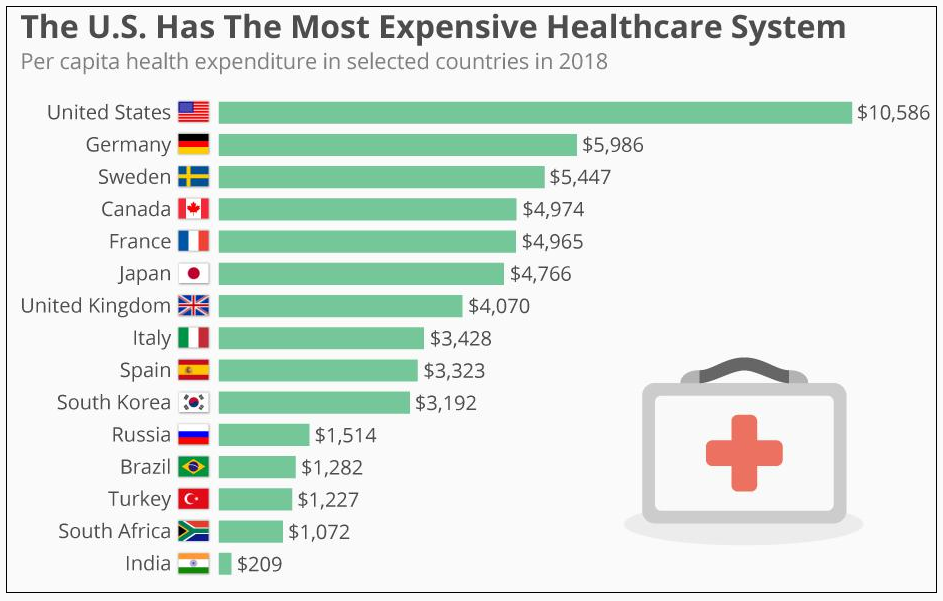
From the presented graphs and images, it is agreeable that Spain tops the list of countries with the best health outcomes and efficiencies (see Figure 1) while at the same time spending less financial resources that other countries (see Figure 2). In terms of efficiency, the government has been putting in place the right mechanisms to ensure that positive results are recorded.
The case of the Spanish health sector reveals that both regional and national apparatuses have been working synergistically to support healthcare reforms ad meet the demands of more patients (Ródenas and Garcés 2017). Privatization of the available health services has made it possible for the government to expand coverage and ensure that all services are efficient and capable of meeting the demands of more citizens.
SWOT Analysis
Strengths
- Spain has a unique model of healthcare whereby public and private players work collaboratively to meet the demands of the targeted patients.
- The designed system of healthcare has a universal coverage that is supported constitutionally.
- The people of this country, including immigrants, had guaranteed right to coverage from both private and public facilities (Ródenas and Garcés 2017).
- The professionals have the relevant skills and receive timely resources that ensure that most of the citizens receive timely medical services (Casanova, Lamura and Principi 2016).
- The developed system of institutions and levels are superior and ensure that all people, including those in rural regions, have access to timely and personalized medical services.
- The government relies on the power of policies and laws to support care delivery processes.
Weaknesses
- In Spain’s healthcare system, private medical insurance remains extremely high in this country, thus making it inaccessible to most of the citizens in the country.
- Most of the national or public hospitals in this country do not have adequate equipment and technologies to meet the medical demands of the citizens.
- Some of the medical professionals in the private sector lack the relevant training and experience. Only those working in the public system have the much needed competencies, thereby creating gaps in the process of care delivery.
- The system does not have adequate mechanisms for responding to most of the emergencies and unanticipated disease outbreaks (Bernal-Delgado et al. 2018).
- The arrangements put in place create a scenario whereby some members of the population have medical demands that are still unmet.
- The MoH is not involved fully in R&D to identify emerging challenges and consider evidence-based approaches and measures that can meet the demands of most of the citizens.
Opportunities
- The first opportunity for the Spanish Health System is the presence of evidence-based practices and cases to borrow from in an effort to improve the speed, nature, and effectiveness of care delivery. For instance, Germany stands out as the best example for borrowing a number of best practices that can help transform the medical experiences and outcomes of more citizens.
- The second one emerges from the nature of medical and healthcare technologies recorded in the world today. The government can capitalize on such systems to design the available systems and procedures and support the delivery of personalized medical services.
- The third opportunity is the presence of like-minded organizations and private institutions that can collaborate with the national government to improve the nature of care delivery.
- Finally, the ongoing research in this sector would be essential to identify most of the existing gaps and consider new ways of improving the resilience and effectiveness of the overall healthcare sector.
- The consideration of these opportunities can guide all leaders and stakeholders to introduce superior practices and ensure the demands of more patients in the country are met.
Threats
- The first threat that the partners and players in this country’s healthcare system are facing presently is the sharp increase in the number of persons affected by these diseases: cancer, cardiovascular illnesses, and stroke (Ródenas and Garcés 2017).
- The second one is the absence of adequate financial resources due to the sluggish rate of economic growth within the past few years.
- The third threat to the effectiveness of the healthcare system is the level of the increasing national debt. Such a challenge will continue to affect the recorded medical outcomes and experiences of most of the citizens.
- The fourth threat is the ongoing COVID-19 pandemic. This outbreak has disoriented and overwhelmed most of the healthcare systems and affected the quality and sustainability of services available to most of the citizens (Legido-Quiqley et al. 2020).
- Finally, the country’s aging population remains a major threat that might disorient the effectiveness and nature of the care delivery systems put in place.
Recommendations
From the above analyses, it is worth noting that Spain is one of the countries with sustainable and properly designed healthcare systems. The government has been relying on the MoH to implement guidelines and protocols that resonate with the demands of the greatest majority. Unfortunately, some gaps exist that make the entire system les effective or incapable of transforming the experiences of most of the citizens (Legido-Quiqley et al. 2020). Various suggestions could be implemented to help address the situation and make the system more resilient and capable of delivering positive results.
The national government can consider the power of modern health informatics to transform the nature of surveillance and ensure that more professionals are prepared for challenges that might emerge in the near future. With some of the citizens and underserved groups lacking health insurance ad support, there is a need for those in power to put proper mechanisms for maximizing insurance cover, improving care delivery processes, and solving most of the recorded gaps (Ródenas and Garcés 2017). The government can also consider and analyze the healthcare systems of different countries that perform effectively and merge the identifiable ideas with the current model. Such an approach will revolutionize the entire system and make it more effective.
Conclusion
The above discussion has identified Spain as one of the countries with sustainable and effective health systems. The existence of private and public models maximizes insurance coverage and provision of timely medical services to most of the citizens. The government relies on the MoH and public institutions to meet the changing demands of most of the citizens. The suggestions outlined above are workable and implementable at the national level. The involvement of all key partners will make it possible for leaders in the system to implement the suggested changes and eventually ensure that more citizens record positive health outcomes or experiences.
Bibliography
Avanzas, Pablo, Isaac Pascual, and César Moris. 2017. “The Great Challenge of the Public Health System in Spain.” Journal of Thoracic Disease 9(6): S430-S433.
Bernal-Delgado, Enrique, Sandra García-Armesto, Juan Oliva, Fernando I. S. Martínez, José Ramón Repullo, Luz M. Peña-Longobardo, et al. 2018. “Spain: Health System Review.” Health Systems in Transition 20(2): 1-179.
Caballer-Tarazona, Maria, and David Vivas-Consuelo. 2016. “A Cost and Performance Comparison of Public Private Partnership and public hospitals in Spain.” Health Economics Review 6(1): 17-23.
Casanova, Georgia, Giovanni Lamura, and Andrea Principi. 2016. “Valuing and Integrating Informal Care as a Core Component of Long-Term Care for Older People: A Comparison of Recent Developments in Italy and Spain.” Journal of Aging & Social Policy 29(3): 201–217.
Legido-Quiqley, Helena, José Tomás Mateos-García, Vanesa R. Campos, Montserrat Gea-Sánchez, Carles Muntaner, and Martin McKee. 2020. “The Resilience of the Spanish Health System Against the COVID-19 Pandemic.” The Lancet 15(5): E251-252.
McCarthy, Niall. 2019. “How U.S. Healthcare Spending Per Capita Compares With Other Countries [Infographic].” Forbes. Web.
Ródenas, Francisco, and Jorge Garcés. 2017. “Toward a Sustainable Welfare and Health System in Spain.” Toward Sustainable Transitions in Healthcare Systems 5(17): 132–52.
This is the Real Spain. 2019. “Spain Health, the Best in the World.” Health. Web.