Introduction
Modern technologies are presently guiding stakeholders in the healthcare sector to improve the quality of care available to more patients. Innovation has become an evidence-based strategy for identifying challenges and addressing them from an informed perspective. The use of scientific developments and innovations could result in superior models for improving people’s health outcomes. The current level of community health performance remains below average due to some of the gaps that affect the process of acquiring emerging technologies. In underserved communities, more citizens find it hard to acquire handheld devices, the Internet, and timely medical guidelines.
The idea of introducing additional policies would be appropriate to ensure that more regions are connected to 4G Internet technology. The guideline will ensure that more people are able to afford handheld devices and utilize them depending on the acquired training programs on technological use. The realization of these strategies would result in a strengthened community health framework in the country.
Scope of Problem
Current literature supports the use of emerging technologies to improve the health outcomes of members of a given community. In successful regions, citizens usually have access to wearable devices, online-based resources, and smartphones that are useful towards supporting their health needs. The complex nature of care delivery allows stakeholders to partner with each other and be able to provide tele-health services (Allen et al., 2021). Pharmaceuticals relying on emerging technologies can inform patients about new or quality drugs. Members of communities can utilize Internet-based services to identify nearest health support systems and design personalized diets depending on their medical conditions.
However, the level of access to most of these technologies presents a major challenge to millions of citizens. Specifically, some individuals encounter unique barriers that make it impossible for them to rely on emerging technologies to meet their health needs. This gap could exist due to a number of issues, such as lack of financial resources, reduced internet coverage, and reduced coordination among the leading medical facilities (Rodrigues et al., 2022). Some communities could lack adequate resources that can make it possible for the members to make informed decisions or manage their medical conditions. The absence of training programs and sensitization efforts to guide more people to start using emerging technologies for positive health outcomes contribute to the list of existing barriers.
Policy Alternatives
Modern technologies are presenting numerous opportunities that medical professionals at the community setting could consider to transform the overall health outcomes of the targeted members. The presence of various barriers makes it impossible for some of the people in underserved regions to utilize such systems to achieve their medical objectives (Long et al., 2018). The absence of proper policy initiatives in the country could explain why some underserved regions are unable to record positive community health outcomes. The failure by the government to introduce coordinated mechanisms to improve healthcare delivery and communication among different stakeholders has led to this problem. The identified issues explain why proper policy alternatives are recommendable to help address some of the barriers to innovation and adoption of technology.
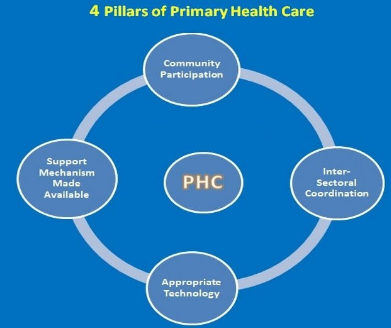
To close this gap, the first policy approach needs to focus on the integrated nature of technologies in healthcare to improve people’s health experiences and access quality services. These 4 pillars of care should guide this framework: appropriate technology, support mechanism, coordination, and community participation (see Fig. 1). This proposal means that the government will offer guidelines for compelling hospitals, community health centers, and government departments to have shared portals and websites. Such platforms will allow most of the community members to identify and access emerging innovations in the fields of technology and science (Willis et al., 2020). This effort will ensure that more people are capable of consulting emerging clinical guidelines and healthcare plans in accordance with their medical problems.
The second policy alternative could revolve around the introduction of 4G technology for supporting Internet connectivity in different regions across the nation. This approach is essential since it helps deliver emerging innovations in the field of technology to improve the level of access to Internet-based resources. Specifically, more patients will be able to connect their computers and handheld devices and learn more about the available information (Allen et al., 2021). This policy approach means more hospitals could share additional insights for managing chronic medical conditions, checking their medical appointments, and receiving virtual health support. This initiative will widen the overall adoption and use of modern technologies to streamline healthcare procedures.
The third policy initiative could be guided by the trends recorded in different parts of the world. Specifically, the government could propose and implement additional laws to compel community-based resources and healthcare centers to educate and guide patients to embrace the use of modern technologies (Rodrigues et al., 2022). These individuals will be able to receive timely updates and instructions for managing their medical conditions or pursuing positive medical practices. Professionals in the field will offer additional guidelines for identifying some of the recorded challenges and opportunities in the field of healthcare (Long et al., 2018). The proposed programs will make it possible for more people to be aware of some of the available technological resources and how they can apply them to meet their changing medical needs.
The fourth policy alternative should revolve around maximizing the use and uptake of technological devices. Over the years, technological firms have innovated and helped deliver a wide range of smartphones and devices that could be adopted to improve community health outcomes. The past decade has been characterized by numerous apps that are becoming resourceful in the management of various medical conditions. Timely policies intended to regulate the prices and affordability of most of these devices, apps, and the Internet could increase the number of people who are able to rely on medical technology (Allen et al., 2021). These achievements will ensure that more people have access to social media platforms, apps, and devices that could result in improved personal health management.
Policy Recommendation
The above sections reveal that barriers to adequate adoption of modern technologies affect the overall health experiences and outcomes of community members in different parts of the country. Specifically, more people from underserved regions are unable to access Internet-based connections and devices that link all other aspects of healthcare delivery. The best recommendation is for the government to support the formulation of a policy that will guide all key stakeholders to collaborate and focus on the best approaches to address some of these barriers (Jonsson et al., 2022).
Specifically, the relevant government agencies should be involved to ensure that all the available community health resources are capable of providing 4G Internet connectivity. The relevant institutions will go further to lower the prices for most of the devices and ensure that they are affordable and capable of supporting people’s healthcare outcomes.
Recommended Resources
The identified policy recommendation is timely and capable of addressing most of the barriers to effective adoption of modern technologies to maximize healthcare delivery and improve patients’ lifestyles. The strategy seeks to increase the number of people in underserved communities who will eventually have access to handheld devices and free Internet. Such beneficiaries will be able to identify most of the available hospitals, management plans for chronic conditions, and tele-health services (Winters et al., 2019). The individuals will liaise with one another and consider how they can improve their overall health outcomes.
To support the realization of the intended community health goals, the relevant stakeholders will have to consider various resources. First, the relevant government agencies will be involved to support the presented idea. Such organizations will offer timely updates about the policy initiative and how it seeks to improve the overall outcomes of most of the community members (Jonsson et al., 2022). Second, all medical facilities, both private and public, in the country need to be involved to share their healthcare programs, clinical guidelines, and disease management plans on their websites. Third, the Internet would become a critical resource for ensuring that more people are capable of connecting their handheld devices and getting the much-needed medical support or guidelines.
Conclusion
Innovation in technology and science is an area that could help improve access to quality, timely, and personalized medical services. The targeted beneficiaries will record positive outcomes and lead healthier lives. The presence of key gaps and barriers explain why the realization of this objective of a community connected health is yet to be realized. The proposed recommendation seeks to compel hospitals and government agencies to support Internet-based practices, devices, and platforms that maximize information access to most of the community members. Such individuals will be able to identify the relevant medical, self-care, or tele-health plan depending on the recorded health problem.
References
Allen, E. V., Haley, J. M., Aarons, J., & Lawrence, D. (2021). Leveraging community expertise to advance health equity: Principles and strategies for effective community engagement. Urban Institute.
Jonsson, F., Carson, D. B., Goicolea, I., & Hurtig, A. (2022). Strengthening community health systems through novel eHealth initiatives? Commencing a realist study of the virtual health rooms in rural Northern Sweden. International Journal of Health Policy and Management, 11(1), 39-48. Web.
Long, L., Pariyo, G., & Kallander, K. (2018). Digital technologies for health workforce development in low- and middle-income countries: A scoping review. Global Health: Science and Practice, 6(1), 41-48. Web.
Mona, M. (2017). 4 main pillars of primary health care. Nursing & Exercise. Web.
Rodrigues, S. M., Kanduri, A., Nyamathi, A., Dutt, N., Khargonekar, P., & Rahmani, A. M. (2022). Digital health–enabled community-centered care: Scalable model to empower future community health workers using human-in-the-loop artificial intelligence. JMIR Formative Research, 6(4), 1-15. Web.
Willis, K., Tuell, C., & Marzilli, C. (2020). Exploring digital health promotion and education in East Texas: Pathways to improving access. Journal of Health Education Teaching, 11(1), 43-55. Web.
Winters, N., Langer, L., Nduku, P., Robson, J., O’Donovan, J., Maulik, P., Paton, C., Geniets, A., Peiris, D., & Nagraj, S. (2019). Using mobile technologies to support the training of community health workers in low-income and middle-income countries: Mapping the evidence. BMJ Global Health, 4(4), 1-10. Web.