Problem Definition
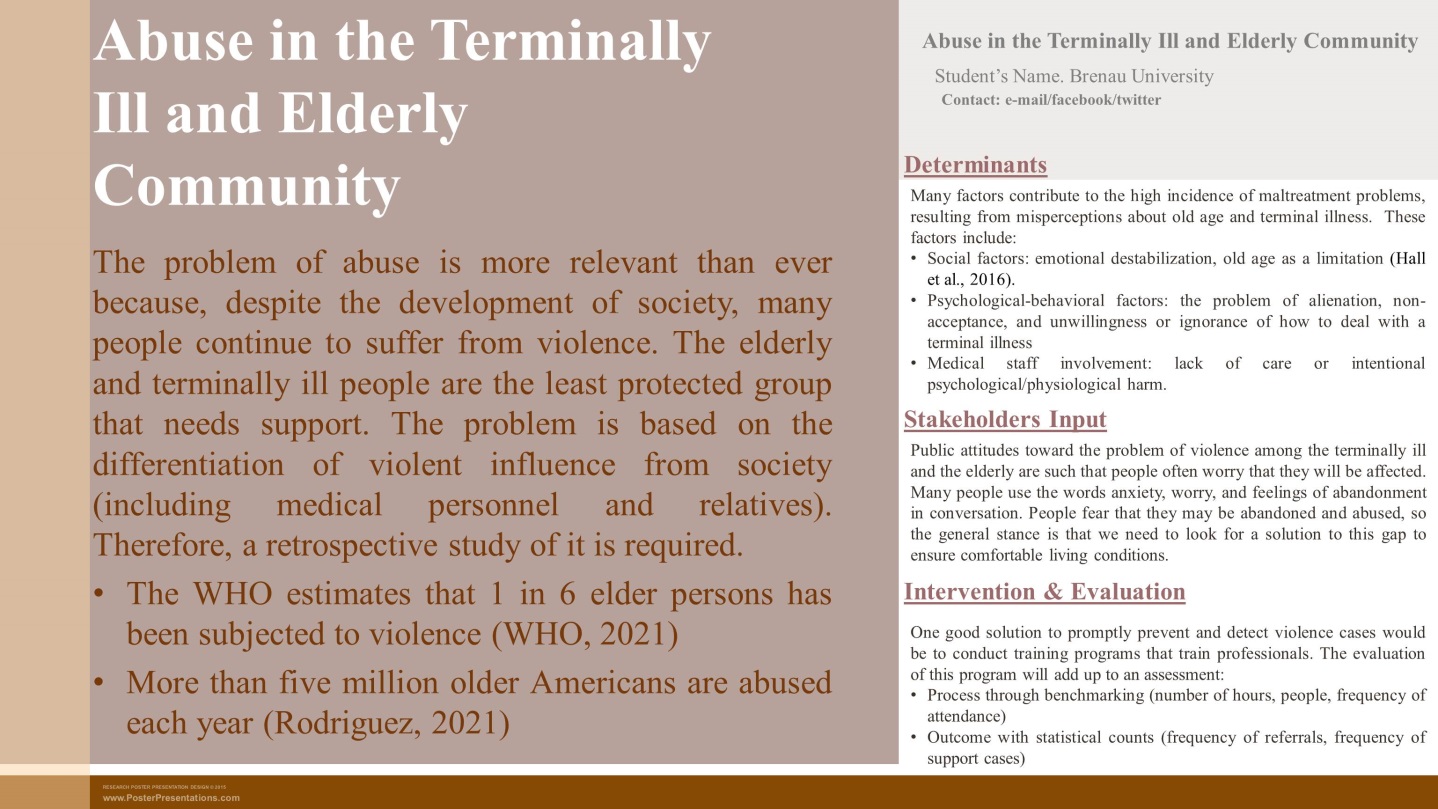
The elderly and terminally ill are the most minor protected groups because of many factors. One such factor is the abuse that occurs at the hands of relatives, medical personnel, and society at large. The abuse problem is acute in the community because it does not always involve physical abuse (Safeguards for medicare patients in hospice care, 2020). Often the abuse is expressed in an emotional or psychological context, which forces humanity to look for new tools to support the elderly and terminally ill population.
Abuse can happen to an elderly person but often affects those who depend on others for help with daily living, including bathing, dressing, and taking medications. The prevalence of abuse is related to various determinants that make for some depressing statistics. More than five million older Americans are abused each year, and the annual loss to victims is estimated to be at least $36.5 billion (Rodriguez, 2021). About 2 in 3 employees of nursing homes or long-term care facilities report that they have committed abuse in the past year (Rodriguez, 2021). According to Families for Better Care, Georgia ranks worst in direct care staffing and 49th in professional nurse staffing (“Georgia elder abuse – nursing home abuse”). Elder abuse is predicted to increase worldwide because many countries are rapidly aging their populations. State structures and social organizations need to put the suppression of violence on the agenda because otherwise, the problem will continue to spread.
Determinants
Many factors contribute to the high incidence of abuse and result from a misperception of old age and an incurable illness. Social factors are considered: society often sees age as a limiting factor that is a burden. It leads to the emotional destabilization of allies: their negativity because of the inability to fix something they pour out on the wards (Hall et al., 2016). In addition, a decisive factor is the stigmatization of incurable illnesses, which forces people to surrender their friends and relatives. Psychological barriers and their overcoming are absent, so people choose the path of violence and alienation instead of the realization of support.
The most frightening and dangerous factor is the involvement of medical staff in violence. Nursing homes or palliative care facilities created for support become places where people no longer feel comfortable. In the case of violence against the terminally ill, the factor of permissibility is the inability of people to resist and obstruct. Medical staff, particularly women, is too close to their wards, making them think they are allowed to behave (Wangmo et al., 2017). They may not be aware that they are harming, but in reality, they are.
Stakeholders Input
The problem of violence is a concern for many people who are aware that it can affect them. Age is a limiting factor, and many adults feel fear about seeking help. I spoke with a healthcare nurse I know, she is 25 years old, and she expresses profound bafflement about what is happening. She is frightened by the lack of monitoring of abusive relationships and would like to see the state pay more attention to these cases. I interviewed several acquaintances who have adult parents and need to be cared for. The sanitariums and preventive care facilities their parents go to provide adequate comfort, but not enough to reduce their anxiety.
Intervention
State apparatuses develop strategies to minimize the damage to prevent abuse. One of the most concerned organizations is the WHO, which suggests that violence will continue to increase unless countries show an interest (World Health Organization, 2021). However, practical methods for dealing with already identified acts of violence would be to send in specialists with specialized training (Alon et al., 2022). Such training would include identifying incidents of violence and specifying them to improve how health and other services are delivered to the elderly and sick population.
Health and education systems should implement the following intervention: a training program with abuse identification and research. This program will enable staff to know how to deal with the elderly and ill, identify their developed problems, and address follow-up issues. Of course, the principles on which the training will be built play a significant role: they should include the concepts of distancing and healthy nursing (“Elder abuse”, 2020). Training to recognize the signs of abusive behaviors will allow institutions to change their patterns of care and eliminate inappropriate staffing based on the results of a statistical study. Such an intervention would be effective because, in the short term, it would identify abuse that has already occurred, and in a long time, it would eliminate the triggers of abuse.
Evaluation
During the implementation of this intervention, three components should be paid attention to how and in what amount of training is done, how many people are involved in the movement, and an unmediated evaluation of the results. An assessment of the process of implementing the intervention will consist of what kind of psychological training the trainer uses (Safe Brantford, 2018). It is necessary to evaluate how much medical staff is involved in the process: how many attend the sessions with what frequency. The main question will be whether the trainees apply the skills they have learned in their practice (Phelan, 2018). It will be assessed by the number of newly identified violence cases, the frequency of direct treatment by older people, and the nature of the violence. It is expected that the final stage of evaluation, the results, will be a retrospective collection of available data that will confirm or refute the cost of the training and the feasibility of the implemented program.
References
Alon, S., Lang, B., & Band-Winterstein, T. (2022). Do training programs promote identification and treatment in cases of elder abuse in Long Term Care (LTC) facilities? Educational Gerontology. Web.
Elder abuse. (2020). National Institute of Aging. Web.
Georgia elder abuse – nursing home abuse. (n.d.). Elder Law Info Lawyers. Web.
Hall, J., Krach, D. L., & Crosby, A. (2016). Elder abuse surveillance: Uniform definitions and recommended core data elements. Atlanta (GA): National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.
Phelan, A. (2018). The role of the nurse in detecting elder abuse and neglect: current perspectives. Nursing: Research and Reviews, 8, 15-22.
Rodriguez, J. (2021). Elder abuse statistics and facts. Gris World Healthcare. Web.
Safe Brantford. (2018). Right now. A Community Strategy to Prevent and Address Elder Abuse. Web.
Safeguards for medicare patients in hospice care. (2020). Medicare Learning Network. Web.
Wangmo, T., Nordstorm, K., & Kressing, R. W. (2017). Preventing elder abuse and neglect in geriatric institutions: Solutions from nursing care providers. Geriatric Nursing, 38(5).
World Health Organization. (2021). Elder abuse. WHO. Web.
Appendix A
Project Poster