Definition
Antibiotics are drugs that are used in the treatment of infections (Lancini, Parenti & Gallo, 1995). The main causative agents of these infections are bacteria alongside other microorganisms. The ability of a microorganism to produce a substance that can hinder the growth of infection was initially used as an antibiotic. Nonetheless, most of the antibiotics used today are synthetic in nature although they have a chemical relationship with organic antibiotics especially in terms of their mode of action.
Antibiotics can also be derivatives of organic substances which may slow down or kill the development of other microorganisms that may cause infections. Hence, antibiotics are designed to selectively destroy harmful microorganisms but not humans.
Uses
There are several uses of microorganisms based on their mode of action. For instance, there are those antibiotics that perform the role of preventing microorganisms like bacteria from synthesizing cell walls in readiness for growth. This type of antibiotic will kill the target bacteria but spare human cells. They have generally been referred cell wall synthesis inhibitors bacteria. On the same note, there are those antibiotics that interrupt the process of protein translation and are referred to as protein synthesis inhibitors. They mainly target the ribosome. Similarly, there are antibiotics that are chemotherapeutic in nature.
They act by stopping the multiplication of cells by hindering the production of DNA and RNA. Finally, competitive inhibitors antibiotics are mainly manufactured. Its function is to interfere with the rate of metabolism, especially of microorganisms.
Example and mode of action
Penicillin is one of the best examples of antibiotics that have been used for a considerably long period of time. It has also been categorized as one of the safest antibiotics to use (Walsh, 2003). It is usually referred to as penicillin G. Nonetheless, this class of antibiotic has its own limitations. For example, its effectiveness is lowered when orally taken since the stomach annihilates it. Moreover, there are some microorganisms that can equally tear it down. It can only hinder the growth of a limited number of bacteria. Due to these shortcomings, there are quite a number of penicillin derivatives that have been developed to improve the effectiveness of the drug.
Mode of action of penicillin
As can be observed from its structure below, penicillin has quite a number of functional groups that perform a myriad of functions when in action. The long carbon chain (R) is attached to carboxylic and methyl groups. Besides, there is the peptide ring attached to the chain.
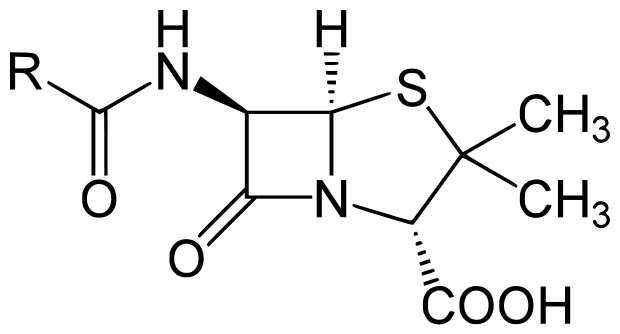
The antibiotic works by hampering with the linkage of the peptide rings which are usually located in the cell walls of bacteria (Walsh, 2003). Once this linkage has been interfered with, the bacteria will become weak structurally making it impossible for bacteria to multiply. However, human cells are not affected by penicillin since we do not have cell walls.
Another example of an antibiotic is tetracycline. It is also a very important antibiotic used to treat infections. Unlike penicillin, they can treat a wide array of bacteria-related infections. This is also the reason why they are referred to as “broad spectrum” (Walsh, 2003).
This class of antibiotics is not recommended for children under the age of eight years since they are known to cause discoloration of teeth in children. In order to maintain the effectiveness of tetracycline, they are usually taken in the absence of food. Patients taking certain types of tetracycline are also advised to keep away from sunlight because they may experience serious sunburn because the antibiotic increases skin sensitivity. Sexually transmitted infections can also be treated using tetracycline antibiotics. Mover, the drug is effective in the treatment of Rocky Mountain spotted fever
Mode of Action of Tetracycline
The structure of tetracycline is shown below.
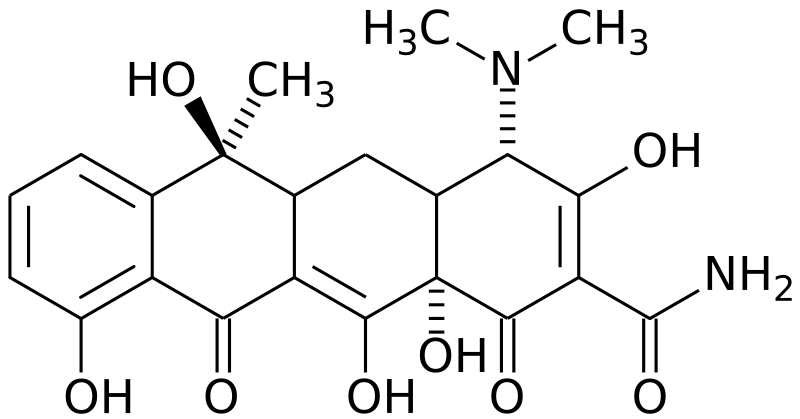
As can be observed, tetracycline has a series of benzene rings and hydroxyl functional groups. The main mode of action of this antibiotic is inhibiting the synthesis of protein by microorganisms. The antibiotic has the ability to hinder the transportation of Ribonucleic acid (RNA) required in the process of protein synthesis. In order to transport amino acids, RNA is paramount. Hence its absence will definitely disrupt the manufacture of proteins in microorganisms thereby hampering their growth.
Although the production of proteins in eukaryotic cells can be inhibited by tetracycline, this antibiotic may not be adequate in terms of the requisite concentration. This is because a viable mechanism to uptake the drug is not present in eukaryotic cells.
Horizontal and vertical gene transmission
It is possible for bacteria to transmit genes that are responsible for antibiotic resistance. This can take place among species or even between species. For example, genes that are resistant to antibiotics like those of staphylococci are usually transferred using plasmids. The latter can be shifted with other species of bacteria such as Enterococcus (Lancini, Parenti & Gallo, 1995). As a result, more genes or a blend if the same is acquired. With reference to vertical gene transmission whereby genes are passed on from one generation to another, the resistant cell which usually remains develops a very strong resistance to antibiotics as the bacterial population grows.
In horizontal gene transmission, bacterial resistance to antibiotics is developed within the same generation. The genes that are responsible for drug resistance are contained in the plasmids. These plasmids can be transported from one cell to another through the process of conjugation. Unlike in the vertical gene transmission, the bacteria do not necessarily be of the same strain or species for transfer to take place. Hence, other species of bacteria can equally develop drug resistance (Walsh, 2003).
Use of antibiotics in Hospitals
The medical practice usually introduces about four to six innovative antibiotics in the market on an annual basis. This is indeed necessary bearing in mind bacterial resistance to antibiotics is ever on the rise and hence the need to contain the situation. Even as antibiotics are being prescribed for use to a myriad of patients every single day, the main challenge remains to be the high rate of resistance to antibiotics developed by bacteria. There are instances when hospitals have prescribed some of these antibiotics to patients with no visible success at all(Lancini, Parenti & Gallo, 1995). Another headache lies in the fact that some of these bacteria that are already resistant to drugs may transmit their resistant nature to other bacteria thereby multiplying the effect.
When antibiotics are unnecessarily used, it precipitates the process of bacterial resistance to drugs. Besides, using antibiotics to treat infections in which the drug used is not effective may also lead to drug resistance by bacteria. Hence, hospitals administering antibiotics on such a basis may as well be worsening the situation. For instance, over 80 percent of infections emanating from the respiratory system are viral related and antibiotics cannot be used to treat them. However, there are several instances when physicians have prescribed antibiotics when patients request for the same or in an attempt to “prevent” other inevitable infections.
In order to alleviate the challenge of antibiotic resistance by bacteria, World Health Organisation (2001) has advocated for the following measures to be taken:
- The most effective antibiotic should be chosen only after identifying the causative agent of the infection ( bacteria or virus)
- It is advisable to make use of antibiotics whose effective range is as narrow as possible so that the target microorganism is attacked within the shortest time possible before it develops any resistance
- Proper dosage should be taken. Incomplete or inadequate dosage of the drug may lead to resistance. Patients ought to stick to prescription instructions to the latter.
References
Lancini, G., Parenti, F. and Gallo, G.G. (1995). “Antibiotics: a multidisciplinary approach”, New York: Plenum Press.
Walsh, C. (2003). “Antibiotics: actions, origins, resistance”, Washington DC: ASM Press.
World Health Organisation (2001). “Antibiotic resistance: synthesis of recommendations by expert policy groups”. Web.