Introduction
The increasing and extraordinary ability of bacteria to resist antibiotics has become a major concern for public health practitioners. It has also been cited as a case of evolution in action which has driven evolutionary scientists to their laboratories with an aim of uncovering how molecules-to-man evolution have come about. This paper discusses the history of resistance, how resistance happens and what action should both the public and physicians take to curb spread of resistance of bacteria to antibiotics.
The discovery of penicillin in 1929 by Sir Alexander Fleming and its wide use during the Second World War was a medical breakthrough that provided the cure for bacterial infections. Today, there are a large number of antibiotics in use which are designed to work on particular bacterial infection. The past 60 years have seen many antibiotics become very important in the treatment of illnesses caused by bacteria and microbes. This is the reason why the twentieth century has seen a rise in the life expectancy. However the increased use of antibiotics has raised another problem for public health. Doctors and health practitioners are increasingly noting that infections such as gonorrhea, tuberculosis, and child ear infections among others have become difficult to treat using antibiotics. This has been attributed to emergence of resilient bacteria and microbes that defy current antibiotics and other microbial drugs and rising use, and misuse of existing antibiotics.
Human use of antibiotics has increased over the years, which have been attributed to development of resistance to many of them. In 1998 alone, US had 80 million prescriptions of antibiotics for human use which amounts to 12,500 tons were made. Agricultural practices accounts for 18,000 tons each year which shows just how much the antibiotic burden to the environment is.
The first discovery of resistance was noted with the bacteria Staphylococcus aureaus’ resistance to penicillin. In 1967, another resistance to penicillin was noted in a remote village in Papua in Guinea. This was Streptococcus pneumoniae called pneumococcus. Penicillin resistant gonorrhea was reported in the American military personnel in south East Asia acquired from local prostitutes around late 1960s which they later brought home. By 1983 a hospital-acquired intestinal infection by bacterium Enterococcus facieum had developed adding to the list of penicillin resistant bacteria which grew very fast. Currently, around 70% of bacteria responsible for many illnesses reported in hospitals, are defiant to at least one the common antibiotics used in their treatment. Some of these bacteria are resistant to all approved antibiotics and the only solution are to fight those using experimental or potentially lethal drugs.
How bacteria become resistance
This happens through natural selection, a theory developed by Charles Darwin in 1800s in his study of ecosystems around the world. Human beings’ immune system fights bacteria by using special cells to invade and shut them down before they are able to infect the body. Illnesses as a result of bacterial infection happen if the bacteria are able to reproduce quicker than the immune system is able to kill them. Therefore, a person with a bacterial infection, have millions of bacteria. Some of these bacteria are resistant to antibiotics based on the Darwin’s random mutations theory. If such a person is given antibiotics, the most susceptible of them to antibiotics dies leaving the resistant ones behind. The bacteria that survive propagate the resistant genes to the next generation creating stronger and nastier bacteria. All this happens when a patient uses antibiotics incorrectly or when antibiotics are used for the treatment of the wrong diseases.
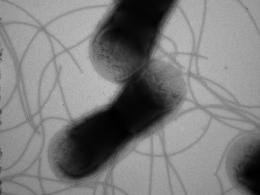
E Coli bacteria, which contains Tn7 found in bacterial strains resistant to antibiotics.
Bacterial resistance happens in four ways according to Antibiotics in action.com 1.
- Through random mutation in the bacterium DNA as explained by Charles Darwin theory,
- Through transformation as a result of one bacterium taking up the chromosomes of another bacterium,
- Through plasmid exchange as the plasmid of one bacterium passes through other bacteria touching them,
- Sharing the resistance to antibiotics mutations as a result of plasmid transfer, and addition of gene cassettes to a bacterium’s chromosomes among others is another way of creating resistance.
Genetically acquired resistance is permanent and inheritable through the process of fusion.
Antibiotic resistance genes are found in the disease causing bacteria as well as in those they live within the same environment such as water, soil, digestive system among others and sharing a symbiotic relationship called commensal bacteria. When humans consumes meat or milk from animals exposed to antibiotics, or plants sprayed with pesticides, the antibiotic and /or resistance bacteria is brought into contact with the one in their digestive system. This contact can allow for transfer of genes from antibiotic resistance one to the one in the human intestines.
Recommended actions for the public and physicians to take to curb resistance
Consumers are advised not to demand antibiotics from their doctors at any one time; never to use antibiotics except when prescribed by their doctors; take antibiotics exactly as they are prescribed by the doctor and complete their full course even if they feel well and never hoard them; observe hygiene by washing fruits and vegetables thoroughly before eating or cooking and avoid raw or undercooked meat or eggs; and avoid antibacterial products such as soaps unless ordered by the doctor.
Physicians on the other hand should observe hygiene by washing hands thoroughly between patient visits; deny unneeded antibiotics demand from patients; prescribing a narrow range antibiotics if possible; ensuring in-patients with multidrug resistance are isolated in the hospital; and keeping tab with the latest information on antibiotic resistance.
Works Cited
Chemheritage.com. Bugs fighting back: basics of bacterial resistance, 2009. Web.
Chemheritage.com. Biological Activity: Resistance in bacteria, 2009. Web.
Georgia, P. Antibiotic resistance of bacteria: an example of evolution in action? 2007. Web.
Lewis, R. The rise of antibiotic-resistant Infections. FDA Consumer Magazine Online (1995).
Todor, K. Bacterial Resistance to Antibiotics, 2008.
Whyfile.org. Microbes: What doesn’t kill makes them stronger, 2009. Web.
Ramanujan, K. Jumping genes’ create antibiotics resistance in bacteria.