Summary
Candidiasis is a wide word that refers to infections of the skin, mucosa, and deep-seated organs caused by a fungus of the Candida type. These infections can occur at any age and are frequently associated with plainly recognizable risk factors for infection. Invasive Candidiasis includes Candida spp. bloodstream infections are also referred to as candidemia, as well as deep-seated infections such as intra-abdominal abscess, peritonitis, and osteomyelitis (CDC). Thus, Candidiasis is a range of infections caused by a fungus that can affect any part of the body.
Causative Agents
The causative agent of Candidiasis is any type of Candida fungus. Under normal circumstances, the fungus causes no illness. However, immune dysfunction, among other things, can encourage fungal overgrowth in the gut and candidemia, both of which can lead to opportunistic infections in multiple organs or invasive Candidiasis (Pappas et al. 18026). Although at least 15 Candida species can cause human illness, the majority of invasive infections are caused by five pathogens: Candida albicans, Candida glabrata, Candida tropicalis, Candida parapsilosis, and Candida krusei. Candida Auris, a formerly uncommon bacterium, has emerged as a serious disease in several regions of the world (Pappas et al. 18). Invasive Candidiasis is a serious healthcare-associated fungal illness caused by numerous Candida species. The most common cause is Candida albicans. However, the incidence of these organisms varies greatly depending on geographical location (Pappas et al. 18026). The illness spectrum of invasive Candidiasis extends from moderately symptomatic candidaemia to fulminant sepsis, with an associated death rate of more than 70% (Pappas et al. 18026). Hence, the main cause of Candidiasis is the fungus that resides on the skin or within the body of a person and, under normal conditions, does not cause an infection.
Pathophysiology
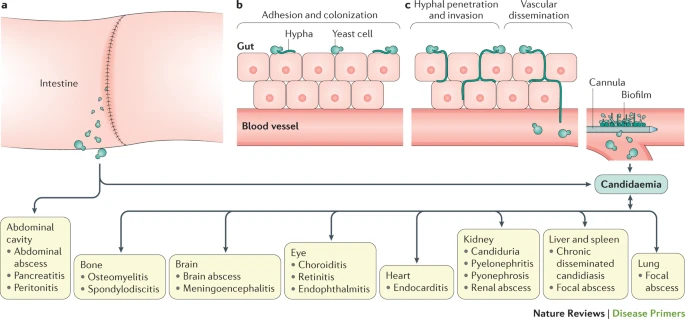
Due to the fact that C. Albicans is the most common cause of invasive Candidiasis, this paragraph will focus on this species. Moreover, this has been the most widely researched Candida species to date, and Picture 1 displays its pathophysiology of it (Pappas et al. 18). Candida can be found on the mucosal surfaces of 50–70% of healthy people (Pappas et al. 18). When intestinal barriers are breached, one example is during gastrointestinal surgery, Candida spp. can enter the abdominal cavity and enter the circulation, causing candidemia.
Treatment
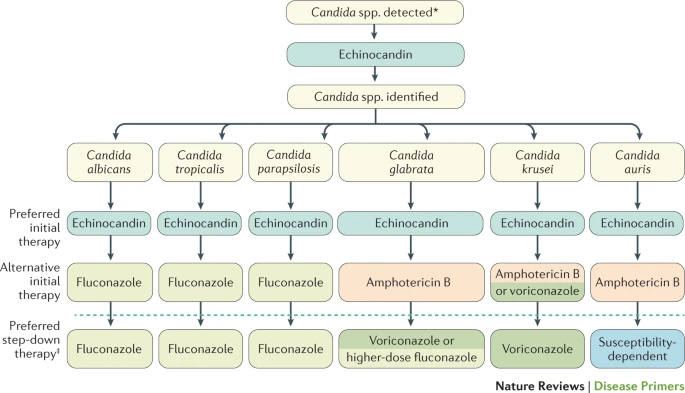
Regardless of the specific species of fungus that caused the disease, Candidiasis can be treated with antibiotics. Early detection of invasive Candidiasis is difficult but critical to good care, and the development of fast molecular diagnostics might increase the capacity to intervene quickly and perhaps minimize mortality (CDC). First-line treatments, such as echinocandins and azoles, are effective, but the advent of antifungal resistance, particularly among Candida glabrata. The resistance to treatment is a cause for concern for the medical community. Picture 2 presents different strategies for treatment. Candida Auris, a recently identified disease, is a multidrug-resistant bacterium that poses a worldwide danger (Pappas et al. 18). Hence, the treatment of Candidiasis is more difficult due to the fungus developing resistance to medication.
Prevention, early detection, and prompt commencement of suitable systemic antifungal medication are key challenges when treating this condition. Since there are few rapid diagnostic ways for invasive Candidiasis, most clinicians rely on routine fungal cultures and empirical evidence to make a diagnosis (Clancy and Nguyen, 19). This method may result in the wasteful use of antifungals in people who do not have invasive Candidiasis, as well as delays in providing effective antifungal therapy to those who are afflicted. These delays in diagnosis and care may result in much poorer clinical outcomes. Hence, difficulties in diagnosing Candidiasis result in the improper treatment or treatment of people who do not have this infection, impacting the drug resistance of this fungus.
Invasive Candidiasis is a new infection that is intimately connected to medical technological improvements and is well recognized as a major source of morbidity and mortality in the healthcare setting (Pappas et al. 18). Invasive illness is frequently the result of excessive or aberrant colonization along with a local or systemic failure in host defenses. Moreover, invasive Candidiasis is not a single clinical issue but rather a condition with a wide range of clinical presentations that can affect any organ since each Candida sp. has distinct features (Pappas et al. 18). Thus, invasive Candidiasis is a complex illness that can affect any part of the human body.
Epidemiology
The incidence of Candida spp. varies greatly geographically. C. albicans remains the most common Candida sp. causing illness in both adult and pediatric populations although the diagnosis of non-albicans candidaemia in both categories has increased in recent decades (Pappas et al. 18026). In most places, the incidence of non-albicans Candida spp. is influenced by variables such as regional antifungal usage patterns, individual patient risk factors, and clonal outbreaks. The latter are outbreaks involving a Candida spp. the molecular strain that is unique in a healthcare setting. In the absence of an epidemic, C. glabrata is the second most prevalent species in the United States and northwestern Europe (CDC). Thus, across the world, infections are caused by different types of candida species.
Pictures
The pictures below show some cases of Candidiasis:
Works Cited
CDC. “Candidiasis.” CDC, Web.
Clancy, Cornelius J., and M. Hong Nguyen. “Diagnosing Invasive Candidiasis.” Journal of Clinical Microbiology, vol. 56, no. 5, 2018, pp. 17-19.
Pappas, Peter G. et al. “Invasive Candidiasis.” Nature Reviews Disease Primers, vol. 4, no. 1, 2018, pp. 18-26.