Introduction
Few medical technologies attract as much public attention as vaccines do. Throughout the history of medicine, physicians, nurses, and doctors have offered a wide variety of treatment formats, and it must be recognized that some of them were indeed dangerous for patients’ health. For example, the excessive use of X-rays for the treatment of soldiers during the war, the use of radioactive surface applications on surgical instruments and very exotic methods of anesthesia still raise some questions. In this regard, it seems even more surprising that a large group of people does not accept the phenomenon of the vaccine, a clinical tool that has been tested by time and levels of evidence-based medicine.
The topic of this research paper is focused on the problem of perception of the vaccine by the general public. Given the complexity of the problem and the potential breadth of the spectrum of reasons why patients refuse therapy, this paper has been divided into several successive sections, covering the theory, statistical references, narrower data on non-recognition of this treatment, and the resulting interpretation of the data. Readers learning this paper will have a good understanding of the phenomenon of vaccination, the relevance of the method, especially during a general pandemic, and the reasons for abandonment.
Theoretical Background
The definition of human immunity and mechanisms of its development is of primary importance in the discussion of the phenomenon of vaccination. Thus, immunity is traditionally called the protective system of any organism that maintains its genetic stability. Such a system protects humans from penetration into the blood of viruses, bacteria, fungi, protozoa, and other pathogens, in combination with poisons, toxins, and allergens from the environment (Hirsch, 2019). However, the immune response of the body does not necessarily have to be directed to external stimuli: the system protects the environment, including from internal threats. Such problems cover mutated and defective cells due to diseases and other pathological processes, as well as products of metabolic decomposition of medicines, ethanol, and other drugs. Summing up the essence of immunity, it must be safely said that it supports the most important one, namely human health.
It is correct to mention further what mechanisms of immunity formation are present in the human body. The first, and perhaps the most important type, is the human innate immunity, which begins to form in the mother’s womb (Offit, 2019). The mother’s body throughout pregnancy and after, during breastfeeding, gives the child a substance rich in blood cells and antibodies. The transfer of such a secret allows the child’s body to build its immunity against foreign agents, which, among others, the mother encountered. A common example of innate immunity is the insensitivity to animal pathogens.
The second type of immunity is artificial, or one that forms the immune system throughout human life. The active category of this type — which is a central part of this research paper — is formed when confronted with new bacteria, viruses, and other infectious agents (Offit, 2019). In such cases, the body must construct its format for fighting pathogens and thus create its antibodies. In combination with the cellular level of control, the body also involves humoral regulation to protect against a foreign agent. It is important to note that if all patients have the same innate immunity, the artificial immunity is unique. In this case, the crucial importance in maintaining health depends on the individual characteristics of the body, the number and quality of previous vaccinations, and the anamnesis.
The Problem with the Vaccine
It is worth introducing that vaccination, or as it has been shown above, active immunization is a widely used method in the medical community for mass prevention of infectious highly contagious diseases: be it viral pathogens such as measles, polio, or hepatitis B, or bacterial pathogens such as tuberculosis, pertussis, tetanus. It is important to understand that the vaccine itself does not cure the disease but only prevents its development through an organized protection system (Treanor, 2016). Hence, the purpose of the vaccine is that the patient’s body is injected with biochemical drugs that contain weakened or killed pathogens of various infections or their parts, antigens that can cause an immune response. The key emphasis should be on the fact that the potential for weakened pathogens is not sufficient for spontaneous disease: their concentration is below a threshold (“Misconceptions,” 2020). Therefore, even if a person falls ill after voluntarily administering a vaccine, it means that the body was most likely not prepared to fight.
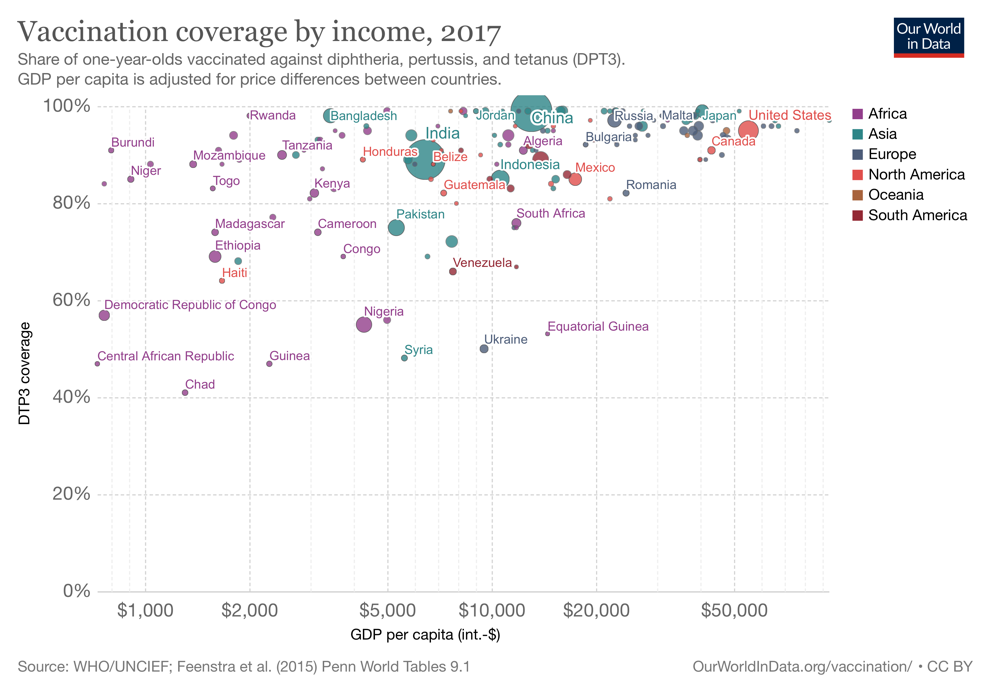
Although the vaccine itself is an economically reasonable, scientifically sound, and medically supported solution to artificial immunization, some patients have traditionally refused to take medicine. The importance of this problem is so high that the World Health Organization even put the vaccine on the list of ten most serious threats to humanity in 2019 (“Ten threats to global health,” 2019). In times of seasonal diseases — be it influenza or VRI — school health centers offer students and their parents a government vaccine that will help the child’s body survive the epidemic, but for a number of reasons, a parent does not approve of such actions. The same applies to adult employees, whose health insurance covers seasonal vaccinations. In other words, the population of developed countries does not have problems with the availability of medical services (as shown in Fig. 1) but still refuses to accept vaccinations.
COVID-19
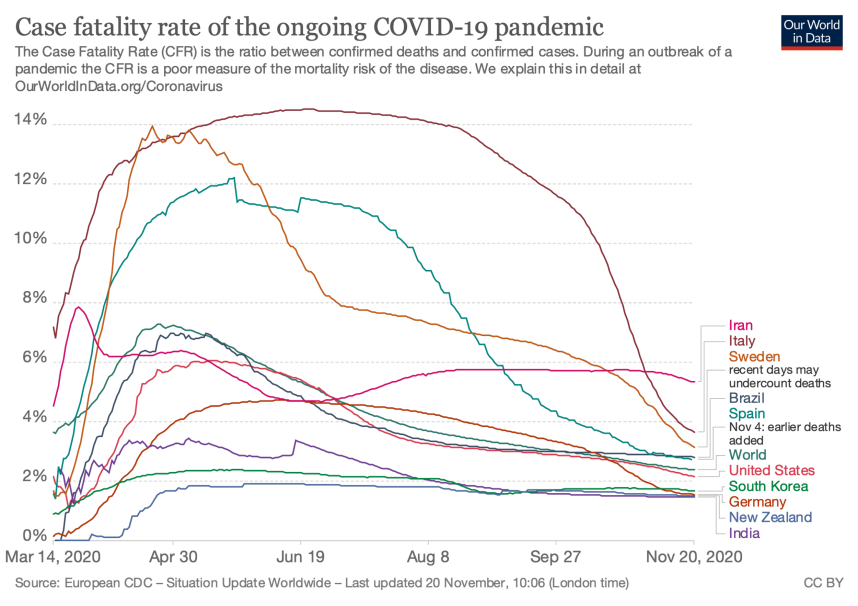
This problem is particularly acute when discussing the coronavirus pandemic, which has become almost the central event of 2020. It is known that the SARS-CoV-2 virus, which is a pathogen of disease, is more likely to affect the lung system and cause progressive lower respiratory diseases, pneumonia, respiratory failure, and distress syndromes. The transmission of this infection is mainly through airborne droplets, but some studies show that contact transmission of the pathogen also occurs (“Coronavirus disease COVID-19,” 2020). There can be no doubt that this highly contagious disease has a much higher mortality index than seasonal influenza, not only because of the nature of the pathogen virus but also because of the failure of the health system to prepare for such a rapidly increasing flow of patients. Thus, according to Ritchie et al. (2020), in the worst of times, COVID-19 mortality could reach 14 percent, although closer to November, these ratings do not exceed 6 percent, as illustrated in Fig. 2. However, SARS-CoV-2 has caused more than 1.3 million deaths since its inception, and this number continues to grow (“COVID-19 coronavirus pandemic,” 2020). Particularly relevant is the threat to vulnerable groups, which include diabetes mellitus, arterial hypertension, and other cardiovascular diseases (Fang et al., 2020). Regardless of the specific numbers, the disease is very dangerous and has the potential to exacerbate the situation even further. However, a solution is already being developed, and it is a vaccine.
The coronavirus vaccine will be a really valuable tool to suppress the number of new cases in the population. It is especially relevant to discuss this during the second wave when, after a summer pause, the dynamics of COVID-19 became shocking again. Thus, there is no guarantee that next year the world will not be affected by a third and then a fourth wave of pandemic, so rapid steps for prevention should be taken as soon as possible. Vaccination — already developed in some countries — will be a serious response to the pandemic and is expected to bring the social, economic, and medical world back to normal.
There is no doubt about that it must be recognized that in the early stages of universal vaccination, some side effects are possible. The reader should understand that the procedure for registering a new medical product is complex and complex, requiring resources of time and money. Although the economic part of the research is hardly under pressure, the lack of time is a significant problem. Many public and private laboratories are interested in developing a drug formula as quickly as possible, so the final stages of clinical trials can be reduced (Graham, 2020). Although this step does not seem to be entirely safe, in fact, the decision is justified by the high mortality rate in the population. It appears that there is a kind of trade-off between potential side effects, which are equivalent to a public health threat, and continued deaths. Choosing the second option can hardly be justified by bioethics, so vaccines are developed faster than usual.
Vaccine Dissidents
It is generally accepted that using vaccines saves lives. The World Health Organization estimates that every year about 2-3 million patients survive on vaccines alone (“Immunization,” 2020). An alternative scenario in which no vaccines have been developed would be worth considering in order to gain an even deeper understanding of the importance of medicines. Historically, the first vaccine, a preparation from smallpox, was developed several centuries ago and during this time is a truly important tool in the fight against the virus. However, if this tool had not been developed, more than 200 million people would have died from smallpox in the 38 years since 1980 alone, according to Vanderslott et al. (2019). These figures are surprising, so the use of the vaccine seems to be more than a reasonable step.
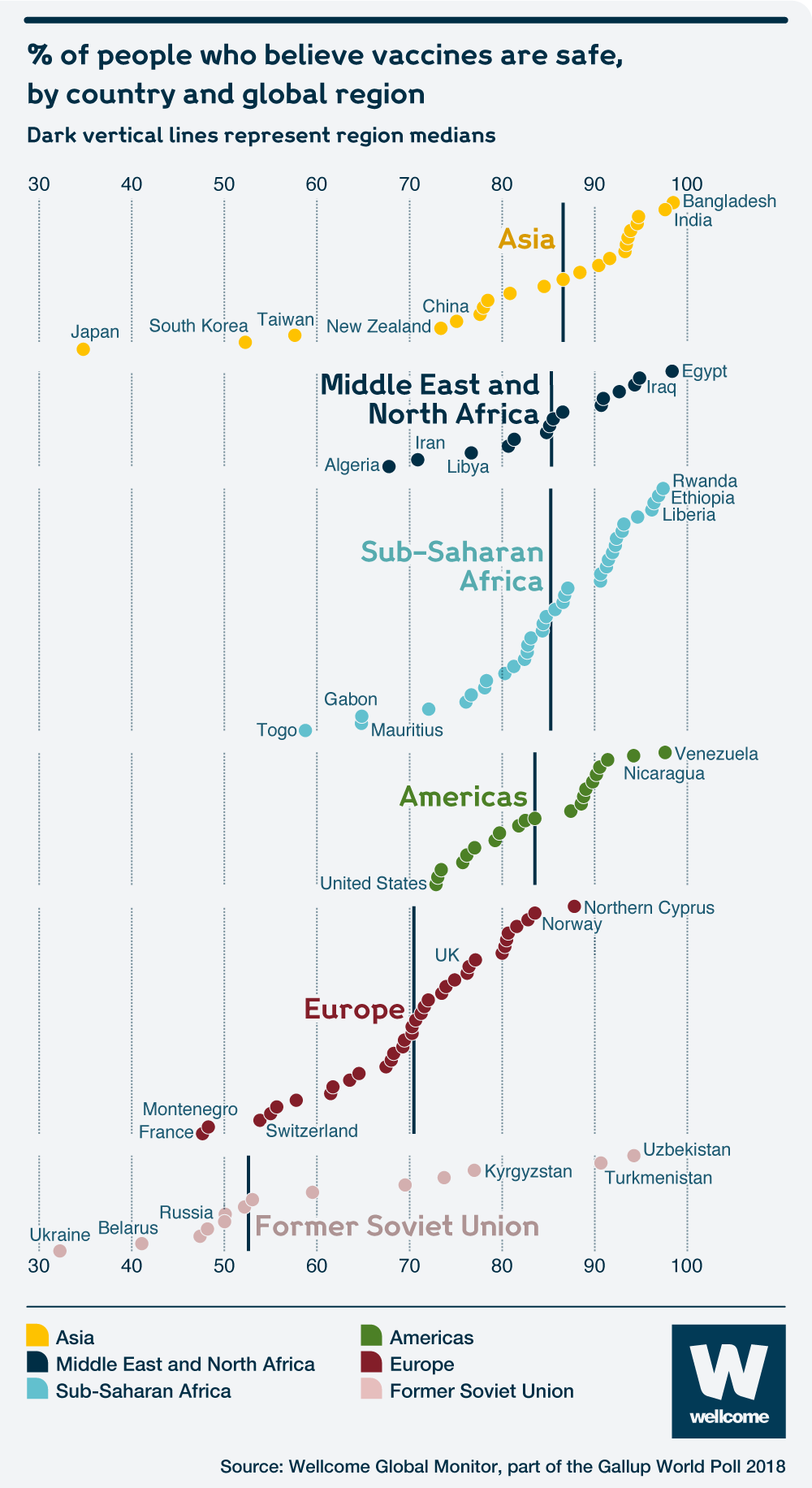
However, failure to take the vaccine is an important public health problem, as it disrupts the prevention system. When a person consciously refuses to inject for any reason, it is equivalent to increasing the threat to their own and public health. Thus, by exhibiting irresponsible behavior, a person damages the entire public health system of the country. In this regard, the data provided by Pesce (2019) showed that the most developed European countries treat vaccination worse than some of the poorest countries on the African continent: this seems even more shocking. According to the statistical survey results of which were published by Pesce, one in three French consider the vaccine dangerous, and one in ten consider it unnecessary for children. A more detailed statistical summary for some countries is shown in Fig. 3.
The statistical picture of vaccination denial in other countries also raises some questions. For instance, over the past decade more than half of the states in the United States have seen that their kindergartens and schools receive fewer vaccines against potentially dangerous diseases such as measles, polio, and hepatitis B (Pilkington, 2019). In particular, Georgia and Arkansas saw declines of more than 6%, meaning that six out of 100 children were not vaccinated against deadly diseases. However, the consequences of this failure occurred immediately, and by the end of 2018, the number of confirmed measles cases among children was twice as high as in 2017 (“Falling vaccination rates,” 2018). In many ways, it was the voluntary refusal of certified vaccination that caused such an increase in the number of long cured diseases.
Narrower statistics allow us to determine that abandonment is primarily among parents. Thus, Blaszczak-Boxe (2016) reported that between 2006 and 2013, the number of pediatricians registering a parent’s refusal of vaccination increased to 87% compared to 75% previously. The ultimate impact of this decision is felt by students, who may not always agree with their parents. According to Morrison et al. (2020), about 24,000 Texas schoolchildren were not vaccinated between 2012 and 2018 because of a voluntary waiver by their parents or their guardians. However, the authors of this study have shown that white people and citizens with higher education are more likely to refuse vaccinations.
Regarding the future vaccine against coronavirus infection, some facts should be further discussed. The study, conducted on a sample of older adults, found that although 86% of mature patients are going to get vaccinated, 14% have not yet decided or will even firmly reject the proposal (Williams et al., 2020). Such data seem to be optimistic overall, although some fears do exist about the older population, which is a category of vulnerability. Another research shows that about 26% of interviewed adults will refuse the coronavirus vaccine (“Ipsos survey for the World Economic Forum,” 2020). Based on these data, it must be assumed that there is an age dependence in the question of vaccination acceptance.
Moreover, the rate of acceptance of the vaccine — including COVID-19 — is clearly divided between some groups. For instance, Malik et al. (2020) showed that Black and unemployed Americans were the most likely to reject the vaccine: although this is not consistent with Morrison et al. (2020). A French survey showed that there is a direct positive correlation with income: the lower the income of citizens, the more likely it is that they refuse to get vaccinated (COCONEL Group, 2020). At the same time, an Australian study links refusal of vaccine to a person’s level of education, arguing that higher levels guarantee the acceptance of a vaccine (Dodd et al., 2020). Thus, there are very clear distinctions in vaccine acceptance, but these differ from country to country. These data suggest that governments should examine the predictors of failure as deeply as possible and conduct outreach to the public.
Interpretation and Search for Reasons
Based on available data, it is possible to construct some judgments about what the main reasons for vaccination rejection are. Such information is of high research and policy benefit, as it allows governing bodies to develop appropriate measures to address subsequent pandemic waves prematurely. Thus, one important reason is the level of education and income among the population, which, however, may correlate. In particular, people with low incomes and low levels of education are the most likely to refuse the COVID-19 vaccination, which means that some of the propaganda should be directed in their direction.
Other trends identified by statistics include age. It appears that the younger a person is, the greater their access to broad information and opinions, and thus the greater the likelihood of commitment to a vaccine targeting dissidents. Older people are less likely to use the Web, so they trust official TV channels that talk about the benefits of the vaccine. In an ethnic context, it has been shown that parents of white schoolchildren are more likely to reject the vaccine, while Black people in the United States as a whole are less likely to accept the benefits of this prevention method.
The main reasons for a voluntary complete rejection of vaccines may be some of the determinants associated with identified trends. Religion is more closely associated with lower education so that many less-educated citizens may refuse vaccinations on religious grounds (Murphy, 2016). At the same time, the lack of biology knowledge that is taught in high school and at higher levels leads some people to believe the vaccine is biologically dangerous (Arora et al., 2018). That is why failure to understand how the drug works makes it easier for people to abandon the vaccine than to understand the clinical dynamics of the substance. Thus, educational level, income level, and ethnicity may be cited as relative predictors of abandonment.
Developing the issue of medical awareness among the population, it should be noted that some ignorance, which originated in the last century, could give rise to dissident ideologies. In particular, it is a voluntary refusal of any vaccination due to a fear of autism. This myth, which became widely known among many patients, was fueled by a misleading scientific publication in which the authors made a direct link between drug injection and the development of autism spectrum disorders in children (Wakefield et al., 1998). In that study, 12 children with autism and autism-like behavior states participated. After studying the intestines of the members and finding some of the measles virus inclusions, the authors concluded that early childhood vaccination was the cause of cognitive disorders. Nonetheless, later research has refuted this paper, and it has been removed from a respected scientific journal. Despite, during the time that it was relevant, a large group of patients, parents, and children became adherents of this idea, and to this day, they refuse the vaccines.
Conclusion
Vaccination has a surprisingly controversial public perception of the medical world. Although this clinical tool has long proven to be highly effective against dangerous pathogens, many people continue to perceive vaccines as dangerous means to their health. This paper has shown that the level of approval of a vaccine depends heavily on certain predictors, including education, income, and ethnicity. Furthermore, most people who refuse the vaccine have religious and profound personal judgments about their decision, but some are convinced that the procedure is dangerous. Timely preventive outreach, broad information, and advocacy should be key strategies to minimize the number of cases of refusal. This is particularly important in the context of the approaching third and fourth wave of the COVID-19 coronavirus pandemic.
References
Arora, K. S., Morris, J., & Jacobs, A. J. (2018). Refusal of Vaccination: A Test to Balance Societal and Individual Interests. The Journal of clinical ethics, 29(3), 206-216.
Blaszczak-Boxe, A. (2016). More parents are refusing vaccinations, but their reasons are changing. Live Science. Web.
COCONEL Group. (2020). A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. The Lancet. Infectious diseases, 20(7), 769-770.
Coronavirus disease (COVID-19): How is it transmitted? (2020). WHO.
COVID-19 coronavirus pandemic. (2020). Woldometer.
Dodd, R. H., Cvejic, E., Bonner, C., Pickles, K., & McCaffery, K. J. (2020). Willingness to vaccinate against COVID-19 in Australia [PDF document]. Web.
Falling vaccination rates pose a global health risk. (2018). Financial Times. Web.
Fang, L., Karakiulakis, G., & Roth, M. (2020). Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? The Lancet. Respiratory Medicine, 8(4), e21.
Hirsch, L. (2019). Immune system. KidfHealth.
Immunization coverage. (2020). WHO.
Ipsos survey for the World Economic Forum [PDF document]. (2020). Web.
Graham, F. (2020). Daily briefing: How desperate measures might shorten the coronavirus vaccine timeline — and at what risk. Nature.
Malik, A. A., McFadden, S. M., Elharake, J., & Omer, S. B. (2020). Determinants of COVID-19 Vaccine Acceptance in the US [PDF document]. Web.
Misconceptions about seasonal flu and flu vaccines. (2020). CDC.
Morrison, M., Castro, L. A., & Meyers, L. A. (2020). Conscientious vaccination exemptions in kindergarten to eighth-grade children across Texas schools from 2012 to 2018: A regression analysis. Plos Medicine, 17(3), 1-18.
Murphy, C. (2016). Key findings on how world religions differ by education. PRC.
Offit, P. A. (2019). Types of immunity. Children’s Hospital of Philadelphia. .
Pesce, N. L. (2019). This is the most anti-vaxxer country in the world. MarketWatch.
Pilkington, E. (2019). US states saw drop-in vaccine rates for children as anti-vaxx theories spread. The Guardian. Web.
Ritchie, H., Ortiz-Ospina, E., Beltekian, D., Mathieu, E., Hasell, J., Macdonald, B., Giattino, C., & Roser, M. (202). Mortality risk of COVID-19. Our World in Data. Web.
Ten threats to global health in 2019. (2019). WHO.
Treanor, J. J. (2016). Influenza vaccination. New England Journal of Medicine, 375(13), 1261-1268. Web.
Vanderslott, S., Dadonaite, B. & Roser, M. (2019). Vaccination. Our World in Data. .
Wakefield, A. J., Murch, S. H., Anthony, A., Linnell, J., Casson, D. M., Malik, M.,… & Valentine, A. (1998). RETRACTED: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet, 351(9103), 637-641.
Williams, L., Gallant, A. J., Rasmussen, S., Brown Nicholls, L. A., Cogan, N., Deakin, K.,… & Flowers, P. (2020). Towards intervention development to increase the uptake of COVID‐19 vaccination among those at high risk: Outlining evidence‐based and theoretically informed future intervention content. British Journal of Health Psychology, 25, 1039-1054. Web.