Palliative care is given to those who are nearing the last days of their lives when providing the best quality for remaining life is more significant than prolonging a miserable life (National Ethics Committee, 2007).
Sometimes even aggressive high quality palliative care does not relieve them of symptoms like vomiting, dyspnoea and severe pain which become refractory to treatment. Keeping them from pain, communicating with them and providing spiritual relief could perhaps work wonders and provide satisfaction to their near and dear ones. Terminal sedation which is a controversial issue, becomes the alternative sometimes and must be resorted to only as per accepted guidelines (National Ethics Committee, 2007).
The home is the best atmosphere for that last journey. However all patients frequently avail of hospital services for treatment and it is natural to conclude that a hospital-based in-patient palliative care unit would be the most sought-after place for their terminal days (IAHPC, 2008). Rapid, intensive and continuous interventions can be provided for patients who are in severe distress; whether physical, psychological or spiritual. The integration of in-patient palliative care service will certainly change the philosophy, policy and care delivery towards terminally ill patients (IAHPC, 2008).
Infrastructure
A palliative care unit needs to have specially trained and clinically skilled professionals at the disposal of the seriously ill patients. The improvement of the patient’s and family’s comfort and their quality of life are in the hands of these professionals (Meier, 2005). At the same time, in the eyes of a manager, the utilization of the health resources should be reduced and the hospital strengthened. Face-to-face clinical incidents should be facilitated by an efficiently designed infrastructure. Routine administrative systems should be operating at a level which allows the clinicians maximum time for palliative care which is time- consuming and labor-intensive (Meier, 2005).
The ‘birth pangs’ of a new palliative unit include “shoestring budgets, lack of support from the health system, lack of understanding about palliative care, and lack of administrative skills by the physicians, nurses, and other clinicians” (Meier, 2005). Palliative care requires sufficiently high quality infrastructure support so as to ensure effectiveness and long term survival of service.
Infra structure includes the “policies, procedures, routines, administrative supports, staffing, schedules, meetings, relationships and billing procedures” (Meier, 2005). The basic requirements for infrastructure would include a mission statement, business plan and budget. Staff positions need to be determined with the nurse manager
heading the list (Meier, 2005). Daily and weekly interactions at meetings are necessary to effectively deal with any situation that may arise. Rounds schedules must be arranged with the clinicians’ knowledge. Ample office space must be found. Filing space for keeping patient-sensitive records safely under lock and key must be arranged (Meier, 2005). Sufficient qualified personnel for maintaining a computerized database and updating data entry and analysis are needed. Computerized billing systems must be perfected. Quality instruments for assessing symptoms satisfactorily must be in place.
Clinical protocols for ventilator withdrawal, methadone conversions and symptom management algorithms are to be finalized (Meier, 2005). Standard order sets for the smooth functioning of the unit must be distributed within the hospital for common practice. Pre-printed progress notes need to be ready. Brochures, posters, business cards and other methods of marketing the services available in systematic fashion would ensure success. Duty coverages should be infallible. Services should not falter for want of staff.
Name of the new unit
The unit that I have planned to set up is a palliative care unit for the Hay’s Urban Hospital. The new unit would be named Hay’s Palliative Care Unit and it is planned to be inaugurated on the 11th of October which happens to be the World Hospice and Palliative Care Day. I have thought up of what the mission statement should be after discussion with the task force. Some articles have influenced us in this matter.
Mission statement
“Let us work together for the improvement of the quality of life of patients and their families through a collaborative effort in dealing with advanced life threatening conditions by innovative palliative care programs, education, research, changing policies, effective communication and spirituality” (IAHPC, 2008; Bycock, 2007; Yingling, 2007).
Our values
Our main aim is to be able to really offer some comfort and attention to the terminally ill patients. In our hands they should feel no paucity of our dedication. The services of our able physicians and surgeons would always be available to the needy. We have sufficient volunteers who would keep the ill company and communicate with them (Meier, 2005). Anyone needing spiritual help would also be duly served.
Planning for the unit
The training at the hospital in New York has given me some idea of making a business plan. I have made several lists for different aspects of the unit with the help of the task force (Meier, 2005)..
Data entry and analysis of the clinical, financial involvement and customer satisfaction outcomes are important components which would allotted to the software engineer who has been recruited (Meier, 2005). He has five years of experience in the same field and is capable of gathering and building a database. Hopefully this is one field which can be considered taken care of.
This unit is planned to be an inpatient and outpatient palliative care unit. The doctors will rotate in the outpatient department. Junior doctors are being posted to do casualty duty all round the clock in shifts. The patients are to be first seen by them and then by the concerned specialist. Nursing staff are being posted for shift duty. Each duty has one recognized team leader. All the nurses would be led by the team leader at times of crises. They in turn inform the manager through their reports (Meier, 2005)..
The palliative care unit has admissions, discharges, the routine ongoing care, charting, assessment sheets, standing orders and other protocols (Meier, 2005). Hay’s hospital has its own internal culture and etiquette. The duty doctors carry pagers and the hospital has a system whereby any doctor can be called for from anywhere in the hospital. It would take only minutes for the doctor to reach the scene of crisis.
New admissions are made all round the clock (Meier, 2005). The duty doctors see the patients and do the needful but all the specialists are just a call away. They take turns to attend calls as is the routine here. Back-up staff are also available for vacations, sick days and any other commitments of the team members. Nurses are present in the wards on their shift duties and no shortage of staff is expected with the present arrangement.
I have built a virtual team of volunteers and trained them to be of service in times of demand. They belong to social service organizations and the convent of nuns attached to this hospital. The core team members have decided in our previous meeting to enhance relationships with this virtual team. Their members are already working in the billing, medical records section, discharge planning, pharmacy and patient relations (Meier, 2005)..
The priest from our chapel and the nuns provide spiritual backing. About two volunteers per patient would be available to provide family support and for any office work. The volunteers would develop a working relationship with the patients and thereby improve the communications with the patient who would be looking out for someone to lean on (Meier, 2005).
Organization chart for nurse manager interactions
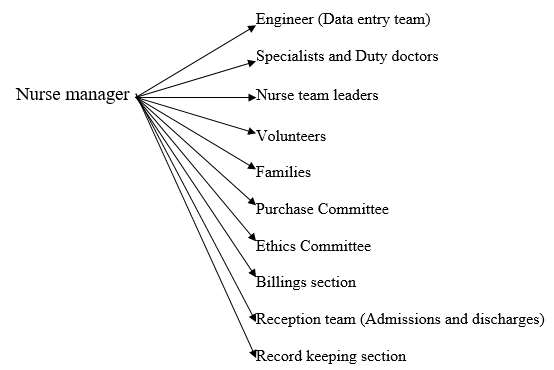
The workload of nurse managers is obvious from this chart. She has hardly anyone to turn to for help. She has to answer for budget variances, labor costs, staffing effectiveness and returns on investment. This budgeting causes her to adjust the number of staff, criteria of workload, patient census, supplies, equipment and revenue (Frisina, 2005). 3 goals are essential for budgeting in surgical services: control of costs, optimization of resources and maximized outcomes. Financial management is the utmost responsibility of a nurse manager (Frisina, 2005). This is a field I have to concentrate on.
Successful efforts in my new job would ensure that there is a direct impact on the Organization’s performance. Quality of care, fiscal stability, patient and customer satisfaction are my targets. Meanwhile, my efforts to empower my team-mates would be strong and I should be able to produce a string of leaders who would assist me in my endeavors and who would be current and future front line managers (Kirby, 2008)
Every aspect of the hospital would come under my purview as nurse manager.
Handling crises would be an added field where my expertise would be frequently questioned. Keeping my shoulders high and above troubled waters would contribute to my efficiency.
Strategies to empower team-mates
The nurse has certain visions when she takes up the reins of an organization. For her work to be efficient and the organization successful, the manager has to carry her team of members to the same frequency that she is operating in. The nurse manager requires strong interpersonal skills like setting goals, delegating responsibilities and empowering her team-mates (Gallo, 2007). Strategies to empower them are manifold.
Modeling the way as a mentoring guide, advisor and coach. (Gallo, 2007)
Leading her team members when the need arises, she models the way for them and allows them to recognize the methods of achieving leadership. The nursing courses do not prepare nurses for these middle management responsibilities (Gallo, 2007). She invites each of them in turn to attend her meetings so that they know what she does to solve crises. She leads by setting an example. Being a mentoring guide to her team mates, she recognizes and helps build their leadership qualities (Gallo, 2007). Internal and external coaching have been found to exceed expectations in producing confidence in 100 % of participants (Kirby, 2008). The leader also encourages them to forgo self interest (Weston, 2008).
She appeals to them in such a way as to generate an emotional involvement and stimulates them intellectually to encourage novel ideas and thinking (Weston, 2008). She fosters collaboration so as to promote common goals. Her ability to share power and information strengthens others.
Developing a pipeline of leaders (Gallo, 2007)
This leadership development by the nurse manager assists the team leaders in rising to the occasion in the event of a crisis. It is a bond of mutual trust. The nurse manager trusts the team leaders to play their roles and this is one stress off her shoulders and she finds time to concentrate on her umpteen other roles. Team leaders also trust their manager in turn enough to approach her in times of need.
Inspiring a shared vision
The nurse manager as the transformational leader has an inspiring vision which she shares with her team members (Gallo, 2007). Their abilities are praised at times to keep them highly motivated. In this manner, both leader and followers are equally and highly motivated and share a common sense of purpose (Weston, 2008).
They would together envisage as to what is to be done in the immediate and far future. The nurse manager manages to kindle their ambitions.
Innovation diffusion
Innovation diffusion which involves in communicating an idea that can change the structure and function of a social system is another technique to empower the staff These innovative ideas must sound better than the present situation and compatible with existing organizational needs (Weston, 2008). An appropriate communication channel must be found to spread the message. Time must be allowed for them to accept the change. They need to be persuaded first; then they have to make the decision, implement and reinforce the change (Weston, 2008). The nurse manager uses this innovation domain to translate the organizational strategies and goals into performance (Gallo, 2007).
Encourage the heart
The good work that the nurse leaders do would be appreciated publicly. This is also a morale booster. The nurse who has put in extra work or one who has chipped in with her talent to save a patient or something which must be recognized as special can be given a rose or a small plaque or applause at a meeting or gathering as sufficient recognition. Team accomplishments may be celebrated together. Hard work or timely interventions must never go unrecognized.
The Wound Team
Reasons for having the wound team
Optimizing wound treatment is essential in a hospital having the surgery department and having a casualty unit too. Hay’s Hospital which caters to a large population has the infrastructure to have a wound team.
The last few decades has seen many innovative technologies in wound healing and care. The use of growth factors, bioengineered skin, topical negative pressure, heat, oxygen, and other technologies have entered wound care healing. (Gottrup, 2004). To function well, these sophisticated techniques require proper wound care and wound bed preparation. It is not the change in the product but the organization of a wound team that increases the healing of a problem wound (Gottrup, 2004).
Considering that the palliative care unit is also being started here, several problem wounds are bound to arise. The wound team is therefore a necessity.
Another reason speaking for the wound team is that the utilization of the multi-disciplinary technique for treatment of wounds has shown a dramatic fall in the number of major lower extremity amputations by 84%. (Gibbons, 1993).
Multi-disciplinary concept
A treatment plan and education are the biggest challenges in wound healing and necessary for product efficacy and cost effectiveness (Gottrup, 2004). Gottrup describes the main factors involved in optimizing wound treatment as “multidisciplinary collaborations, structuring of the treatment process (development of expert functions), and education and training of health care personnel and patients.”
Multidisciplinary teams are now found for all kinds of wounds and burns. Some hospitals adopt the multi-disciplinary team for all wounds and some have different teams for different wounds like burns team, diabetic foot team and so on.
The wound team here would be a multidisciplinary department treating all types of problem wounds. (Gottrup). The system of having junior doctors on duty all round the clock helps start the treatment as soon as the patients arrive and continued by the senior doctor in the team. The senior specialists in the surgical, dermatological, plastic surgery and medicine units would be the team leaders and all the other members of the team would come under them.
All the specialists in the surgical department comprising of the ear, nose and throat specialist, orthopedic specialist and the eye specialist would be members of the team and see the patients when called. Considering the involvement of many specialties, this team would be an “independent, integrated, multidisciplinary expert area.” (Gottrup, 2004).The other members would be the nurse leaders and volunteers who help the patients.
Standardized treatment for chronic or problem wounds would conform to the treatment protocols at the national level. However for complicated non-healing wounds without a diagnosis, a centre conference treatment plan would be evolved with the team leaders involved. Follow-up and evaluation would be done.
There would be an outpatient clinic and inpatient ward with beds for only wound patients. Researches would be conducted to discover outcomes, patient satisfaction and cost effectiveness. (Gottrup, 2004). Education and training would involve Educational Developmental projects, study in different societies, and training programmes for doctors and nurses (Gottrup, 2004).
Frequent interactions would take place with the team leaders, nurse leaders and volunteers in the form of meetings of the Wound Team where healthy criticisms and good work are both analyzed with me as the coordinator.
Purchases would be made as per protocols under the supervision of the team leaders and me.
The issue of the two nurses
The two would be cordially invited to my office for a discussion. I would inform them how supplies are ordered in a matter-of-fact manner not considering the heated debate. Once they have understood the method involved, I have to elaborate on the repercussions of such an ugly incident in the hallway. They have to be reminded of their responsibility in the noble nursing profession. That they are leaders in their own respect should be pointed out to them.
They are the people in the forefront of the dedicated services that the profession offers. How their ‘saviors’ behave would affect the confidence level of the sick patients. They would tend to be more miserable. Keeping calm and explaining things in a warm way and getting them emotionally involved, the erring nurses would be persuaded to maintain the dignity and composure befitting a member of the profession. Had it been only a matter of knowing how supplies are ordered, they should have come to me.
Self respect is essential even before respect for a colleague. Whatever the issue, the service package that the profession or the hospital offers is a coordinated effort of all the members of the team. The nurses who are team leaders in their own respect are to be looked up to by the patients, families, cleaning staff, volunteers and whoever works in that place. Seeing their leaders in such a pitiful situation would stop them respecting nurses as a whole and the organization.
By the time I am through, I expect them to look up to me as a person who can be approached in times of crisis. They should refrain from such an incident in future.
References
Bycock, Ira R.; (2007), “To Life! Reflections on Spirituality, Palliative Practice, and Politics”, American Journal of Hosp Palliative Care 2007; Vol. 23, No.6, Pgs 436-438.
Frisina, Michael E.; (2005), “Peer presence: Tips for top challenges”, Nursing Management, Pg.81.
Gallo, Kathleen; (2007), “The new nurse manager: A leadership development program paves the road to success”, Nurse Leader, Vol 5, Issue4, Pgs 28-32.
Gibbons GW, Marcaccio EJ, Burgess AM, Pomposelli FB, Freeman D, Campbeli D, Miller A, LoGerfo F. Improved quality of diabetic foot care, 1984 vs. 1990; reduced length of stay and costs, insufficient reimbursements, Arch. Surgery, 1993, 128, pgs 576-581.
Gottrup, Finn; (2004), “Optimizing wound treatment through health care structuring and professional education”, Wound Repair and Regeneration Vol. 12, no. 2, Pgs 129-135.
International Association for Hospice and Palliative Care, (2008), “Inpatient palliative care in a general hospital’, IAHPC.
Kirby, Karen K.; (2008), “Nurse Manager Development Beyond the Classroom”, Nurse Leader, Vol 6, Issue 2, Pg 44-47.
Meier, Diane E. and Beresford, Larry; (2005), “Infrastructure Supports What Is Most Important in Palliative Care”, Journal of Palliative Medicine, Volume 8, Number 6.
National Ethics Committee, (2007), “The Ethics of Palliative Sedation as a Therapy of Last Resort”, American Journal of Hospice & Palliative Medicine® Volume 23, Number 6, Pgs.483-491.
Weston, Marla J.; (2008), “Transformation Leadership at the National perspective” Nurse Leader, Vol 6, Issue 4, Pgs.41-45.
Yingling, Julie and Keeley, Maureen; (2007), “A Failure to Communicate: Let’s Get Real About Improving Communication at the End of Life”, American Journal of Hospice and Palliative Medicine, Vol. 24, No.2.