How to Obtain Necessary Approval
Before choosing the best procedures to follow in getting the approval to undertake the health research, I would investigate all relevant health bodies involved in the implementation of the health plan and find out all legal frameworks governing the process. After doing so, I would seek approval from the relevant organizations and ensure they are onboard concerning the implementation of the program. Getting approval from the organizations would be pivotal to the success of the program because the health administrators at the facility could provide resources needed in the formulation and implementation of the health plan (Brännström & Boman, 2014). As part of the approval process, I would also apply for ethical consent before undertaking the health management plan from the relevant ethical committee on health. Collectively, these processes would outline the main steps I would take in getting the necessary approval for the health plan.
Description of Current Problem, or Issue
Research has shown that there are increased incidences of readmission for patients who have undergone treatment for congestive heart conditions (Desai & Stevenson, 2012). Part of the reason for the high readmission rates is the lack of proper education concerning post-discharge health management. Indeed, as Desai and Stevenson (2012) say, many patients are unaware about what to do after leaving the hospital. Adib-Hajbaghery, Maghaminejad, and Abbasi (2013) delve deeper into this issue by exploring the possible causes for the high incidence of readmission in acute care facilities and say that ineffective education is the main reason for this outcome. In other words, patients do not understand the right steps to undertake across the full continuum of care, from the hospital to the home. In this regard, there is a deficit of information concerning what patients should do when they leave hospital. Consequently, patients should be educated about what they should do, from the time when they leave the hospital up to the time they recover fully in their homes. At their homes, having the right education about what to do to manage their health would help them to monitor and maintain a good health. The education could also spread into active intervention for ambulatory patients who have exhibited signs of decompensation (Desai & Stevenson, 2012).
Detailed Explanation of Proposed Solution
Traditionally, the heart failure clinic has been the venue for chronic heart failure management (Desai & Stevenson, 2012). While its role, in this regard, is essential in health management, there should be a deliberate effort to reengineer its purpose to serve a broader mandate of educating patients about what they should do after discharge. Consequently, we propose to reengineer the role of the acute care clinic to educate patients about health management. To highlight this strategy, we would use the model described by Desai and Stevenson (2012), which complements the role of the integrated heart failure treatment center as the focal point for intermittent, chronic heart failure management, which not only helps to treat such conditions, but also educate patients about what to do concerning the management of their health conditions. The diagram below represents this model
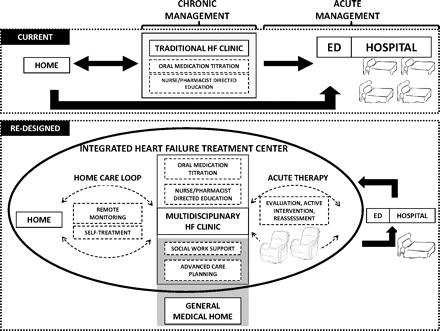
To understand the proposals made in the above diagram, it is important to understand that HF means heart failure and ED means emergency departments. The top-tier model represents the traditional framework of treating acute heart conditions. It also represents the current model for managing heart conditions. However, the redesigned model of doing the same uses a re-engineered approach of heart failure treatment, which not only focuses on the acute care setting, but also includes a “home care loop,” which involves monitoring patients in their homes.
Therefore, the redesigned model of chronic heart management differs from the traditional approach of the same by having a tighter linkage to home surveillance. It also includes options for active treatment as a plausible alternative to hospitalization. This proposal could significantly reduce the incidence of readmissions that result from the poor management of heart conditions. More importantly, it would be easier to eliminate all individual barriers to effective care by increasing patients’ level of education. Furthermore, the same strategy would shift existing health priorities of cardiac care management from inpatient care management to outpatient care management, thereby providing an alternative approach of managing heart conditions.
Rationale for Selecting Proposed Solution
The above-mentioned proposed solution for the current health problem exemplifies a unique way of reducing hospital readmissions that result from the ineffective care of patients suffering from heart-related problems. It is unique because it involves the minimum deployment of health resources since it only involves an expansion of the health management scope.
In other words, instead of only focusing on providing health solutions to admitted patients, it also seeks to educate patients about the best care management strategies to use at home. In this regard, it recognizes the interconnectedness of health issues, at home and at the health facility. With the decline of financial resources available to treat patients, the proposed strategy outlines a cheaper way of reducing the health burden on health facilities by reducing the incidence of hospital readmissions. In this regard, the return on investment for the proposed plan is high because the proposed solution has returns that are greater than the investments made.
Evidence from Literature to Support Proposed Solution
According to Agboola, Jethwani, Khateeb, Moore, and Kvedar (2015), educating patients about how to take care of themselves when they leave the acute care setting not only helps them to improve their health outcomes, but also assists them to reduce the levels of anxiety associated with having heart problems. Different researchers have investigated the relationship between improved education standards and positive health outcomes and found that although their relationship is controversial, the positive health returns of education could easily outweigh its financial investments.
David Cutler and Adriana Lleras-Muney (cited in The National Bureau of Economic Research, 2016) are some authors who hold this opinion. The consensus among these researchers is that education shares a linear relationship with positive health outcomes (The National Bureau of Economic Research, 2016). Many researchers have used this reason to quantify the effect of education on positive health outcomes by saying that four years of education could lead to five years of reduced mortality (Agboola et al., 2015). In this paper, we have used the same justification to highlight the role of education in reducing the incidence of hospital readmissions.
Description of the Logistics for Implementation
Part of the problem facing the implementation of public health programs is the poor execution of plans (Brännström & Boman, 2014). Particularly, failing to understand the different roles of participants in the implementation process is often a commonly overlooked problem in the implementation strategy (Brännström & Boman, 2014). The proposed health management strategy would have an elaborate role assignment plan that outlines unique duties that each project participant would play. To explain the logistics of implementation, we answer the most important questions regarding program implementation as outlined below:
When and how will the change be integrated into the current organizational structure, Culture and Workflow?
I would integrate the change in the organization structure after consulting with the hospital administrators and getting their approval. The integration process would happen by changing the organization’s policies and procedures concerning care delivery. Stated differently, instead of prescribing drugs and discharging patients at the end of the care process, the nurses and physicians would be required to educate them about what they need to do at home, and notify them of the risks they expose themselves to, by failing to follow the recommendations given. Proper education would allow them to understand the need for taking their medicine on time and getting proper rest (among other procedures that they need to observe during their recovery). To integrate this new approach of health management in the organizational culture, there should be an appointed health administrator to spearhead the change and make sure that every health practitioner follows the new proposal.
Who will be responsible for initiating the change, educating staff, and overseeing the implementation process?
The senior health care counsel would oversee all operations that concern the implementation of the program proposal. His responsibilities would mainly revolve around planning and implementing evaluation activities. He would also be required to coordinate program efforts and be responsible for evaluating program activities, including planning and budgeting (Centers for Disease Control and Prevention, 2012). For purposes of making sure that the proposed plan has an effective design to blend well with the existing organizational operations, the senior health care counsel would also have to develop program objectives and work with other consultants to make sure there is an adequate stakeholder buy-in when implementing the plan (Centers for Disease Control and Prevention, 2012). Comprehensively, the role of the senior health care counsel would be pivotal to the successful implementation of the health plan.
Resources required for Implementation
The main resources required for the implementation of the proposed plan include hospital staff, educational materials, assessment tools, technology, and financial resources. The hospital staff would be the most important resource for the implementation of the plan because they are the first point of contact between the patients and the hospital. Furthermore, they are the main implementers of the plan because they have a duty to educate the patients about the best health management strategies to observe after discharge.
Nurses also have a strong interpersonal relationship with the patients, which is an asset in monitoring the progress of the patients during recovery. Furthermore, they are bound to make effective follow-ups of the patients’ progress since they are likely to have a good access to the lives of the patients. The educational materials that would be useful during the implementation of the health management plan would be vital for cross-referencing purposes, as patients could easily refer to the information contained in the pamphlets to manage their health.
The educational materials would also contain bullet points that highlight key issues that the patients need to consider in managing their health. Assessment tools needed in the implementation plan would ordinarily include questionnaires and survey tools to monitor and evaluate the patients’ progress before and after they are educated about the best health management strategies to use. Lastly, the financial resources needed for the implementation plan would mostly relate to the cost of educating the patients and training the hospital staff to do so.
References
Adib-Hajbaghery, M., Maghaminejad, F., & Abbasi, A. (2013). The role of continuous care in reducing readmission for patients with heart failure. Journal of Caring Sciences, 2(4), 255-67.
Agboola, S., Jethwani, K., Khateeb, K., Moore, S., & Kvedar, J. (2015). Heart failure remote monitoring: evidence from the retrospective evaluation of a real-world remote monitoring program. Journal of Medical Internet Research, 17(4), 101-09.
Brännström, M., & Boman, K. (2014). Effects of person‐centered and integrated chronic heart failure and palliative home care. PREFER: a randomized controlled study. European Journal of Heart Failure, 16(10), 1142-1151.
Centers for Disease Control and Prevention. (2012). Introduction to Program Evaluation for Public Health Programs: A Self-Study Guide.
Desai, A., & Stevenson, L. (2012). Rehospitalization for Heart Failure Predict or Prevent? AHA Journals, 126(4), 501-506.
The National Bureau of Economic Research. (2016). The Effects of Education on Health.