Abstract
This paper aims to review and study the issue of professional and job burnout in nursing practitioners, as well as to identify the primary causes and the main consequences of this problem. The adjustments that have been made to the system and management have resulted in a new strain being placed on the nursing staff, which has led to a decline in the quality of treatment, safety, and overall satisfaction experienced by patients in this hospital. It is a reasonable assumption to make that some of the causes of the nursing shortage at the hospital are due, at least in part, to the fact that nurses are exhausted, stressed out, and burnt out. The particulars of the capstone project, as well as the connected organization, are related to the need for relevant data on nurse burnout, distress, and psychological challenges to be carefully analyzed. These concerns need to be considered using a more universal or international frame of reference. At the same time, it is inconceivable to disregard the thought that COVID-19 has significantly influenced the healthcare systems, especially the nursing departments. This is due to the fact that it has become impossible to deny the existence of COVID-19. Furthermore, the paper has a particular objective of assessing and analyzing various methods and current approaches that are used presently to prevent and address nurse burnout. Moreover, the author endeavors to emphasize a concrete technique that can be potentially implemented for combating nurse burnout in the medical-surgical department of the associated hospital. In fact, the impacts of burnout on nurses are detrimental, and an integrated program of mentorship and mindfulness is intended to help mitigate those effects.
Introduction
Burnout is a kind of stress that is caused by one’s place of employment. It is characterized by a condition of physical or psychological tiredness, a feeling of diminished achievement, and a loss of one’s identity. It is possible to develop burnout as a response to protracted or persistent job stress if one is exposed to stress in the workplace for an extended length of time. Professional burnout can occur among specialists in the field of nursing, which can subsequently lead to diminished job engagement and turnover. Concerning the associated organization, in the past few years, especially during the COVID-19 pandemic, there was a rise in nurse turnover in the Intercommunity hospital. The changes in the system and management have caused different stress on nurses and gave a lower patient care, safety, and satisfaction rate in this hospital. It is feasible to assume that some of the reasons for the shortage of nursing in the hospital are due to nurses being tired, stressed, and burned out. The effects of nurses’ burnout are negative and must be addressed by an integrated mentoring and mindfulness program.
Review of Literature
Basics of Nurse Burnout
The relevance of the research on features of emotional burnout syndrome in nurses is connected with widespread manifestations of this pathology among medical workers. Intensification of professional activity, expansion of the list of duties, high workload, and nurses’ round-the-clock commitment cause the development of psycho-emotional tension. Medical professionals are entrusted with significant responsibility for human life and health, which entails the risk of burnout.
The nature of the professional activities of nurses in the therapeutic and surgical departments is distinct, which may include the degree of burnout manifestation. Thus, this issue exists in Medical-Surgical units in a small intercommunity hospital. This is due to a large number of patients, and nurses in small hospitals perform essential work and receive burnout.
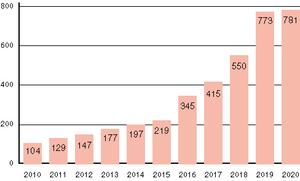
The research on this topic is extremely important because burnout among medical professionals has consequences not only for the individual professional but also for the patient and the business. Since nurses constitute the largest cohort of healthcare professionals, a multitude of studies has been conducted to investigate the factors that contribute to their burnout and the interventions that have been attempted to combat it (Buckley et al., 2020). Although research into the causes of nursing burnout is increasing, there is still a need to research ways to prevent it and therapy (Dynamics of The Number of Publications on The Topic of Emotional Burnout in The Period 2010–2020, Buckley et al., 2020). Thus, the literature is absent a single classification of the reasons for burnout and the ways of struggling against it are insufficiently investigated.
However, researchers have focused on the causes of burnout in nurses. Several of these factors include the working atmosphere and the perception of the nurse. One study found that the involvement of the nurse in care activities, including decision-making, ambiguity regarding treatment, and a lack of job clarity, were variables that contributed to higher nurse burnout (Buckley et al., 2020). Other elements that may contribute to the emergence of burnout include being exposed to issues such as sorrow, grief, misery, and death; furthermore, feeling hopeless, delivering care that is pointless, and experiencing general moral anguish (Buckley et al., 2020). The reduction of burnout experienced by nurses has the ability to lead to improvements in both the well-being of nurses and, ultimately, the quality of care provided to patients.
Nevertheless, there is another point of view, Garcia et al. (2019) argue that in addition to the standard factors that provoke burnout, it is essential to focus on ineffective cooperation, failing organizational systems, and health workers’ psychological and physiological overburden. In the current world, ensuring the safety of patients is recognized as one of the most important challenges. This is due to the fact that the quality of patient care often depends not only on broken systems, inefficient organizational procedures, and inept management but additionally on the actions of medical professionals (Garcia et al., 2019). Changing behaviors will need these professionals to have improved educational backgrounds (Garcia et al., 2019). It is predicated on the notion that errors in patient care are a result of human failings in relation to communication, collaboration, and psychological wellness among health workers.
Although each of these elements contributes in its own unique way to the quality of care that is delivered to patients, occupational well-being, anxiety, stress, and emotional exhaustion are all influential determinative factors. It has been hypothesized that there is an established connection between low wellness and moderate to substantial degrees of burnout, which in turn leads to poor patient safety and assistance mistakes (Garcia et al., 2019). Burnout is an ailment that is specifically linked to a work engagement environment due to the workplace stress that health and education laborers are unceasingly under (Garcia et al., 2019). Thus, this pressure is primarily associated with contact with other people, which makes burnout a disease that is mainly correlated with employment conditions.
Risks for Nursing Personnel
When referring to the typical threats that healthcare workers can face, they are influenced by tiredness throughout their shifts. As a result, they are unable to provide patients with quality treatment and may endanger the whole healthcare system as a whole (Garcia et al., 2019). Patient safety is influenced by various elements, including those that are individual, interpersonal, and organizational and dependent on both material and human resources. Burnout is contingent on these qualities, including physical and organizational aspects and human relationships; as a result, there is an inherent connection between these and other related concepts (Garcia et al., 2019). There is a correlation between the existence of burnout in health workers and an increase in the risk to patients (Garcia et al., 2019). Furthermore, there is a link between high degrees of burnout and things that are external to the individual, such as a heavily loaded job, long working hours, and negative interpersonal relationships (Garcia et al., 2019). Therefore, preventing professional weariness is a critical tactic for enhancing the level of safety provided to patients.
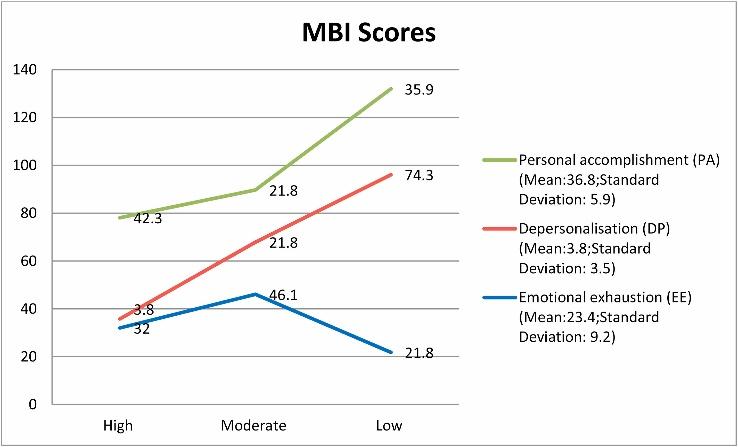
In contrast to the common threats suggested by Garcia et al. (2019), there is the concept of Jun et al. (2021), which relates nurse burnout to their individual mental health and general organizational outcomes. The emotional tiredness, depersonalization, and decreasing personal achievements that are hallmarks of burnout place a considerable load on the physical and mental well-being of individual nurses (Jun et al., 2021). It is extremely necessary to investigate nurse burnout within the context of the healthcare system, given the rising body of research demonstrating the negative effects of burnout on nurses, patients, and institutions. Contextualizing burnout as an institutional and communal occurrence provides a larger perspective that is important to treat nursing burnout (Jun et al., 2021). Generally, burnout has been considered an individual problem (Jun et al., 2021). As a consequence, emotional exhaustion in nurses can be considered a form of professional stress that affects not only nurses but additionally patients, corporations, and society as a whole.
Individual Consequences of Burnout for Nursing Specialists
Fatigue in nursing is a detrimental and severe condition that impacts not only the people who are affected by it, but the facility in which those nurses work and the patients they care for. It is estimated that as much as 50% of the nursing industry is suffering from burnout, which may lead to negative personal consequences, dysfunction at work, and even possible danger to patients (Kelly et al., 2021). It is reasonable to state that burnout is a factor in personnel quitting their professions, given that burnout is defined by three typical symptoms: weariness, depersonalization or pessimism, and decreasing personal achievement (Kelly et al., 2021). Individuals who have reached their burnout point may become restless while doing their utmost to provide treatment for patients whose prospects of recovery are low.
This view is supported by Jun et al. (2021), as the personal repercussions of emotional issues and tiredness among nurses can lead to various complications, including interpersonal ones. Misanthropy may manifest itself in the form of uncharacteristically negative actions, poor communication with colleagues, and eventually discourtesy toward coworkers in the case of the practitioner who has reached burnout (Kelly et al., 2021). When caregivers are burnt out, they have the perception that they are not fulfilling their professional tasks to the maximum levels, they lack the enthusiasm to do their jobs, and they have reduced job-related self-esteem (Prevalence of Burnout, Kelly et al., 2021). Hence, it is possible that the emotional toll taken on healthcare personnel, particularly nurses who deal with patients as they pass away, will have an effect on the nurses’ individual feelings.
Financial Aspects of Nurse Burnout and Resilience Indicators
As a result of the stresses associated with their jobs, nurses may have a diminished sense of personal success and an overall lack of pleasure, which may ultimately lead them to quit their jobs. It is estimated that the loss of a nurse abandoning their position is linked to substantial financial costs, ranging from $11,000 to $90,000 per caregiver, with approximately to $8.5 million in related broader costs (Kelly et al., 2021). These costs are in addition to the disruption that is caused to the care that is provided to patients (Kelly et al., 2021). Therefore, as per the financial details, job stress in the healthcare sphere can provoke the emergence of unnecessary expenditures and excessive uncertainty.
In this situation, scholars were capable of examining the resilience indicators among nurses to assess the quantifiable data. In fact, the ratings of nurses’ resilience are improved if they have been working as nurses for longer, engage in work tasks, and wish to remain in their role (Jun et al., 2021). In addition, the resiliency of nurses who participate actively in their job by joining a professional group is likely to grow (Jun et al., 2021). As a result of the significance of recognizing and lowering the rate of burnout in the industry, companies have a responsibility to systematically assess burnout and well-being. It is compulsory in order to comprehend the influence on employee turnover and find solutions to the problem.
Nurse Burnout in Emergency Departments
With regard to burnout and tiredness in nurses and caregivers, it is obligatory to emphasize the aspects of the issue in emergency departments since this healthcare workplace condition is different in comparison to others. Since patient treatment may be unexpected, emergency departments are recognized for their high-stress workplace (Sexton et al., 2021). Due to this setting, burnout among nurses in the emergency room is believed to be prevalent, and burnout levels continue to rise, which is detrimental to the profession (Sexton et al., 2021). Workplace climate, stress management, and a lack of supervisory support are all major causes of burnout and compassion fatigue in the emergency department.
In this scenario, it is additionally feasible to compare the mental consequences of tiredness in the emergency department between nurses and physicians. Evidence shows that emergency room nurses are more susceptible to experiencing burnout and compassion exhaustion, as well as reduced compassion satisfaction (Sexton et al., 2021). The contradictory evidence suggests that, unlike nurses, emergency department physicians had a high degree of burnout in the emergency department (Kelly et al., 2021). Nonetheless, the prevalence of victimization among nurses is greater than among medical specialists, suggesting an elevated incidence of disengagement in nursing (Sexton et al., 2021). As high burnout percentages are a sign of high turnover, hospitals must tackle stress and burnout inside the emergency department in conjunction with physician burnout.
Nurses’ Opinion on Burnout
Concerning the review of literature related to the field of burnout in nurses, it is necessary to discuss separately the factors associated with nurse burnout and their relative prevalence. In 2018, among nurse practitioners who reported quitting their present jobs, 31.5% mentioned burnout as the reason for their departure (Shah et al., 2021). These conclusions were identified according to the results of a statistical examination of survey data collected from cross-sections of more than 50,000 registered nursing specialists (Shah et al., 2021). Both are spending more than 20 hours each week and operating in an environment similar to a hospital were related to an increased risk of burnout (Shah et al., 2021). Participants who had left their jobs or considered quitting them due to burnout indicated a difficult work environment and insufficient personnel as the primary reasons for their departures (Shah et al., 2021). Nurses are an important subset of clinicians who possess a wide range of competencies, including the ability to promote health, prevent illness, and provide direct treatment.
Another perspective is expressed by Garcia et al. (2019); that is, healthcare managers may demand better performance in each practice area because of the increased duties and responsibilities placed on nurses. The increased burdens of healthcare organizations and physicians have resulted in an increase in the expectations put on nurses, which has, in turn, had a detrimental impact on the working environment for nurses (Garcia et al., 2019). It is of extreme significance that people have a better understanding of the job-related objectives and the variables that lead to burnout in nursing staff across the United States. This is due to the fact that nurses possess a diverse set of skills, play a critical role in their teams, and account for a significant portion of the workforce in the healthcare industry.
Shah et al. (2021) indicate that mental and emotional stress and the stressful nature of their work environment related to caring for patients who are ill or approaching the end of life are common among nurses. Professionals working in health care are typically regarded to be among the groups most at risk of experiencing burnout (Shah et al., 2021). There is sufficient evidence to support the claim that some features of the working environment are linked to burnout among nurses (Shah et al., 2021). A number of issues have been identified as contributors to nurse burnout, including increased workloads, an absence of assistance from the administration, and a lack of teamwork between nurses and doctors (Shah et al., 2021). Hospitals and other institutions with a reputation for providing high-quality nursing services have demonstrated the importance of reforming aspects of the workplace environment, particularly education-related support (Shah et al., 2021). Hospitals can cooperate with academic medical centers for educational assistance in this situation.
Furthermore, it is necessary to determine and assess the factors of influence linked to workload and working shift hours among nursing practitioners in the United States of America. The amount of time worked each week by caregivers was positively related to recognizing burnout as a cause for quitting their post or contemplating leaving their position (Shah et al., 2021). However, the dominating function at work was not shown to have any association with this phenomenon (Shah et al., 2021). According to the findings of certain studies, employees who work longer hours and cannot get enough sleep are more prone to burnout (Shah et al., 2021). Others have pointed to a significant connection between lack of sleep and mistakes made in the course of providing medical treatment to patients (Shah et al., 2021). Burnout is characterized by a number of different symptoms, one of the most prominent of which is emotional weariness. Work overload hours and a lack of sleep are likely to increase this tiredness. In general, nurse practitioners keep reporting feeling burned out in a range of practice situations throughout their job-related tasks and duties.
The Issue of Nurse Burnout in Medical-Surgical Departments
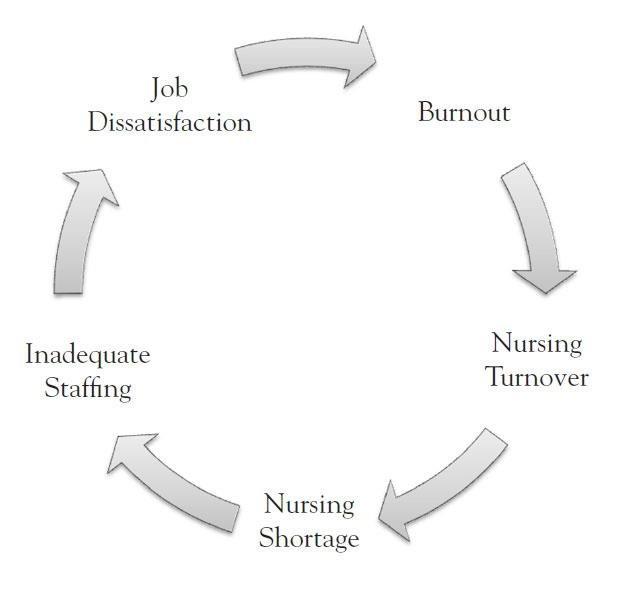
According to the background of the paper, it is compulsory to emphasize and discuss the aspects of the issue of nurse burnout in medical-surgical departments. In general, the selected topic relates to the organization, which is a medical-surgical unit in a small Intercommunity Hospital, since medical-surgical nurses can also be seriously affected by the negative consequences of tiredness and burnout. The turnover rate of nurses is a global problem that affects all nursing specialties (The Nursing Burnout Cycle, Phillips, 2020). However, the problem is especially severe in medical-surgical fields, which require critical numbers of exceptionally qualified nurses due to the high nurse–patient ratio values, utilization of point-of-care systems, and stressful conditions of employment (Phillips, 2020). Since the tasks of healthcare personnel in medical-surgical departments are believed to be of high priority, it is evident that unaddressed turnover and burnout in nurses can lead to unpleasant consequences.
With the help of analyzing the outcomes of research articles, it is possible to identify a statistical interpretation of the importance of nurse staffing and the ability to preserve a positive psychological atmosphere. As per the results of a recent study, more than half of the individuals employed by medical-surgical departments indicated heavy workloads and plans to quit their present post (Phillips, 2020). In addition, this conclusion is consistent with the final findings of the study. The amount of burnout experienced by the sample as a whole ranged from mild to high (Phillips, 2020). Based on the results, the likelihood of a nurse quitting their present position is proportional to how much they believe their workload contributes to feelings of exhaustion and burnout (Phillips, 2020). These outcomes should be taken into consideration by nurse managers when formulating initiatives to enhance the working environment and increase nurse retention.
Topic Objectives and Analysis
Preventing and Combating Nurse Burnout
The specifics of the capstone topic and associated organization are connected to the need to properly analyze relevant data regarding nurse burnout, distress, and psychological difficulties. These questions should be discussed from a general or global perspective. At the same time, it is impossible to ignore the notion that COVID-19 had a major impact on the healthcare systems, including nursing departments. In this case, it is compulsory to integrate an assessment on how nursing practice and, consequently, nurse burnout were influenced by the rapid dissemination of the virus. Furthermore, in terms of the topic objectives and analysis in the paper, it is required to encompass the evaluation of various separate methodologies that describe ways of addressing and preventing nurse burnout. Hence, different scholarly articles are to be examined, considering the need for identifying appropriate solutions for nurse burnout avoidance or tackling.
Stress in Nurses During COVID-19
The widespread of the COVID-19 coronavirus illness has made it more probable for nurses to have symptoms that pose a risk to their health, wellness, and capacity to continue working. Due to the accelerated spread of the illness in late 2019 and early 2020, several healthcare systems were unaware of the situation (Arnetz et al., 2020). Thus, they had to rearrange to supply critical care unit spaces, respirators, and personal protective gear for individuals as well as healthcare professionals.
As a result of the epidemic, nurses have been forced to contend with a combination of situations that pose a risk to their health and capacity to complete their job-related tasks. Publications in the articles from several of the COVID hotspots throughout the globe described considerable weariness and physical pain as a result of extended working hours while wearing face masks and other safety clothing (Arnetz et al., 2020). In addition, the studies highlight the fear of being contagious as well as the mental discomfort that the external pressure causes in nurses (Arnetz et al., 2020). The juxtaposition of physical and mental pressure placed on a nursing profession that was already under a significant amount of strain has evolved into a defining characteristic of the COVID-19 epidemic.
In fact, it is feasible to underline the issues of personnel training and development in nurses in relation to their preparedness for extra pressure. A problem that has been noticed in various publications and that is a factor in nurses’ poor psychological health is the absence of proper training, specifically among nurses who were dispatched from other specializations (Arnetz et al., 2020). During the COVID-19 outbreak, concerns about the workplace have been noted, and challenges with treatment plans and supplies have been identified (Arnetz et al., 2020). It was one tangible approach that may assist in maintaining nurses safe and lessening their anxiety of being infected.
This concern could be alleviated by equipping nurses with proper personal protective gear. During the pandemic, healthcare facilities were unable to give confidence to nurses to address the strain they are facing, encourage one another, and provide recommendations for workplace adjustments (Arnetz et al., 2020). As a consequence of the urgency and lack of time, institutions and care managers were unable to comprehend the causes of stress. This approach was essential in order to identify viable organizational actions that would ensure the health, productivity, and well-being of caregivers.
COVID-19 and Nursing Interns
With regard to issues in nursing during the pandemic and the lack of sufficient education and preparation on how to cope with similar emergencies, it can be stated that intern-nursing students were especially affected. Due to the impossibility of healthcare and medical facilities to provide care and treatment for everyone, intern-nursing students were included in the emergent and other departments’ teams. A nursing internship training serves as an overview of a professional career, easing the transfer from the position of a student nurse to that of a registered nurse or licensed practical nurse. It offers intern students a fantastic chance to put knowledge into practice and enhance their nursing abilities before graduating, which is a major benefit of the program (Eweida et al., 2020). The nursing students get their clinical instruction in a number of different critical care units during the duration of this practicum semester.
Internship students had, for the most part, battled with the dangerous obstacles of their accelerated medical training, and they were burdened with severe attacks of stress. Experienced nurses, on the other hand, had no identical or similar problems. In the instance of COVID-19, the reasons for this anxiety extended beyond the practical internship experience. Instead, it was caused by the fact that the hospitals were being fulfilled with diagnosed and suspected patients at the same time that its medical supplies were becoming dangerously low (Eweida et al., 2020). In particular, students developed sentiments of mental upheaval as they witnessed their classmates being ill, quarantined, or even passing away (Eweida et al., 2020). In fact, this issue caused the learners to acquire additional psychological attacks. It is possible that the intern-nursing trainees can become more susceptible to psychological discomfort as a result of the mental pressure caused by the challenges with which they are presented.
In the aftermath of the COVID-19 outbreak, students who were enrolled in nursing internships were experiencing devastating attacks of stress. In summary, female interns reported experiencing greater levels of psychological discomfort linked with COVID-19 than their male counterparts did (Eweida et al., 2020). The difficulty of ensuring the learners’ health during the COVID-19 period was unique to the field of clinical nursing education and was not confronted by any other academic program (Eweida et al., 2020). In general, while other academic establishments had completely transitioned to the use of virtual learning, which was inapplicable for clinical training, students who were studying to become intern nurses had to work in healthcare facilities.
COVID-19 and Nursing Turnover
Concluding the theme of the major negative influence of the COVID-19 outbreak on nursing and nurse burnout, it is feasible to emphasize the correlation between the pandemic and nursing staff turnover. Furthermore, it should be noted that nursing staff turnover rates are connected to burnout in nurses since emotional and psychological problems can become a vital impacting factor on the potential decision to leave among nurses. The number of patients in critical condition, the lack of information available about the illness, and the high mortality rate associated with the disease all contribute to the mental strain that nurses experience.
The epidemic made the previously concerning problems of frustration, exhaustion, and turnover among nurses considerably worse. This statement can be assessed as particularly relevant in case it is stated that these problems existed before the pandemic. The high turnover rate of nurses has been named a problem for the whole healthcare system, despite the fact that it can be justified as being a choice and early departure from nursing work (Falatah, 2021). The turnover rate of nurses may be increased due to either organizational factors or professional factors, with the former being the more significant factor since it contributes to the already existing nurse shortage (Falatah, 2021). There is a correlation between the desire to turnover and a number of unfavorable outcomes, including prescription errors, accidents, and stress injuries (Falatah, 2021). In addition to this, there is a possibility that it contributes to higher overall expenditures within the healthcare system as a result of the effect it has on both monetary and personal resources.
One of the areas of the healthcare industry that was severely affected by the pandemic was nursing. Nurses are a significant part of the healthcare provider community and spend a substantial amount of working time directly with patients. Prior to the outbreak, nursing was considered to be the profession that had the highest intention rates of employee turnover (Falatah, 2021). Before and during the COVID-19 epidemic, several academics strongly emphasized the alarmingly high percentages of nurses who intended to leave their jobs (Falatah, 2021). The COVID-19 pandemic has caused an increase in the amount of tension, anxiety, and panic that nursing personnel experience around the possibility of catching the virus (Falatah, 2021). These psychological aspects may be reduced if nurses obtain advanced training in the care they provide for patients, which would also lessen the likelihood that nurses may leave their jobs. Moreover, nursing supervisors and other leaders should offer mental guidance and assistance to nursing staff members in order to minimize the number of nurses who leave their jobs.
Measures and Approaches for Preventing and Combating Nurse Burnout
The first strategy to combat nurse burnout is to enhance the nursing work environment by creating and implementing a cultural change toolkit. This will help to make the nursing profession less stressful overall. The toolkit is a program that provides knowledge and resources for treatments centered on published research and inspires positive modifications in practice (Adams et al., 2019). It is possible to design and execute a culture change toolkit inside a department by integrating the many different suggestions that may be found in the relevant literature.
Intervention programs relating to meaningful acknowledgment, collaborative decision-making, and greater leadership participation and support are included in the toolbox. When taking into account the practical application, there was a drop in both the projected turnover and burnout ratings among nursing staff throughout the phases of prototyping and testing, which was a positive development (Adams et al., 2019). After conducting testing, it was determined that the decrease in overall burnout levels had a statistically significant impact, and over the whole of the project, no resignations arose among the staff nurses (Adams et al., 2019). In this particular instance, the program’s objective is to improve the perspective of the clinical practice setting to lessen the amount of burnout experienced by nurses.
At the same time, it is feasible to identify a number of constraints and drawbacks associated with this specific method. In the first place, this initiative does not take into consideration any of the individual circumstances that can put a nurse at risk for burnout. Furthermore, since the research was exclusively completed in a single department, the findings of the study cannot be generalized well enough; hence, more validation is necessary (Adams et al., 2019). Since avoiding burnout is crucial, it is debatable whether or not this strategy can be equally effective in both addressing the problem of burnout among nurses and preventing its occurrence.
Another methodology for dealing with the prerequisites and aspects of nurse burnout and emotional instability is to adopt positive emotional skills interventions as a conception. A growing number of healthcare facilities have started to provide wellness programs for their nursing staff in an effort to combat nurse burnout (Cheung et al., 2020). On the other hand, the majority of these approaches and solutions are geared toward alleviating inadequate states, for instance, anxiety, tension, and despair (Cheung et al., 2020). The distinct and autonomous function that positive emotion plays in fostering adaptive coping mechanisms in the context of stress is being highlighted by an increasing body of data (Cheung et al., 2020). Among this scenario, it is conceivable to provide a strategy for the prevention of burnout in care providers and nurses (Cheung et al., 2020). This approach is an initiative that teaches people techniques that were shown to be effective in the past, with the specific goal of increasing pleasant feelings. This intervention, which focuses on developing positive emotional skills, has been used effectively with various groups and may be adapted to meet the needs of nurses in critical care.
In contrast, this method of coping with the results of nurse burnout or abolishing the elements that can cause burnout to occur has disadvantages. When compared to self-guided treatments, supported interventions can necessitate more time, money, and effort to spread; thus, these are major disadvantages of such initiative types. Moreover, it is compulsory to consider that results of emotional skills interventions are difficult to be measured and analyzed, especially in a quantifiable manner, due to the probable deviations in feedback among nurses. Finally, it is complicated to comprehend whether this approach would be totally suitable for nursing specialists in medical-surgical departments.
The subsequent methodology that can be found useful in terms of preventing nurse burnout or abolishing the risk of its consequences’ emergence is to elaborate a social and individual work lead mindfulness-based intervention. The findings of the research suggested that respondents experienced both personal success and emotional tiredness as a result of their labor (Wampole & Bressi, 2020). The nurses felt that the intervention had the potential to foster improved emotional control not exclusively in the workplace but outside of it (Wampole & Bressi, 2020). Training social workers in mindfulness practices might be a resource that has not been fully used yet for increasing patients’ emotional well-being and the quality of treatment they provide. Practices based on mindfulness have been investigated for their potential to avoid and lessen the negative consequences of anxiety and burnout in a variety of professions, notably nursing (Wampole & Bressi, 2020). These strategies were shown to have a positive effect on general practitioners and a reduction in depersonalization and mental anguish among healthcare workers (Wampole & Bressi, 2020). Hence, the promotion of self-care and well-being among a variety of healthcare and nursing professionals can be anticipated.
Alternatively, these programs should be reinforced by workplace supplies and policies that encourage participation and respect mindfulness practices as an essential component of promoting effective patient care. At the same time, this approach can be considered a feasible and useful one in the setting of the medical-surgical department. Nursing professionals in medical-surgical departments frequently provide care and nursing services to individuals in serious conditions, for example, after a stroke, or prepare people for complex surgical procedures. In this situation, social worker education on mindfulness techniques can be beneficial as they provide practical assistance for specialists related to their emotional and psychological aspects and perception. Increased awareness of attitudes, emotions, and behaviors, as well as an altered sense of oneself and a broader appreciation of life, may all be fostered via the practice of mindfulness.
In addition, it is possible to assess the elaboration and implementation of a specific course to promote and improve self-care for nurses to address or prevent burnout. Strategies for lowering the risk of burnout include adopting healthy behaviors such as eating well, getting sufficient sleep, and being physically active. The authors of the study designed an education plan for caregivers and other personnel of healthcare teams to address the issue of burnout and discuss various ways of coping with the stresses of both work and life (Couser et al., 2020). The findings revealed a high incidence of burnout among nursing professionals and a low level of confidence in obtaining adequate levels of nutrition, rest, and movement (Couser et al., 2020). The purpose of the course is to offer nurses and other practitioners the chance to explore a variety of subjects that are linked to healthy habits. Moreover, it is designed to exchange ideas that may be used to handle stress and avoid burnout. In fact, this technique can be combined with the solution of incorporating a social worker education on mindfulness into a single and connected system for nursing specialists.
For medical-surgical departments in hospitals, it is feasible to recommend the application of a separate mentorship program for internal communications. Mentorship is the inspiration, instruction, or guidance provided by a mentor, who is a teacher or advisor to a less-experienced individual. The study emphasized the development of a mentoring program based on evidence for newly registered and certified nurses recruited into medical-surgical departments at community-based facilities (Krofft & Stuart, 2021). According to the findings of the study, the nursing leadership of the hospital encouraged the project implementation to create a stronger assistance system for prospective nursing practitioners (Krofft & Stuart, 2021). In general, this system was completed in an effort to increase nurse retention. It should be noted that the medical-surgical units had to deal with a large number of process modifications in a short amount of time as part of the reaction to the pandemic (Krofft & Stuart, 2021). As a consequence, the need for an expanded support network for the recently recruited nurses grew exponentially and urgently.
Global Approach to Address Nurse Burnout
Concerning the global scale of addressing the issue of nurse burnout, it is reasonable to underline institutional- and national-level practices. To ensure the safety of both nurses and patients, the authors of the study suggest developing a comprehensive strategy for the mandatory implementation of staffing ratios across the country (Schlak et al., 2022). It is recommended that staffing ratios be adopted with monitoring from the federal government and cooperation from legislative bodies (Schlak et al., 2022). The working environment that promotes clinician well-being is the same working setting that permits providing high-quality care to patients (Schlak et al., 2022). Burnout, disengagement, and their respective implications should all be reviewed on a regular basis to monitor the efficacy of improvements made to the work environment. Furthermore, data on nursing resources, including personnel, skill levels, and workplace culture, should be released to the public (Schlak et al., 2022). Thus, patients may select where they receive their medical care depending on nursing-sensitive characteristics. It is possible for healthcare institutions to display their dedication to the well-being of nurses by changing their attention to the elimination of systemic barriers in working environments.
Leadership, Nurse Burnout and Turnover
Nursing productivity may be increased with the help of a fully-qualified leader. Job strain among nurses and turnover rates are influenced by leadership styles at hospitals and other healthcare facilities (Pishgooie et al., 2019). There is a strong correlation between leaders who use a transformational or transactional approach and those that cause their employees to stress on the job and predict high turnover (Pishgooie et al., 2019). Leadership characterized by a lack of interference was associated with greater work stress and a higher likelihood of employee departure (Pishgooie et al., 2019). Nursing staff burnout and turnover may be mitigated via the use of transformational and transactional categories of leadership styles (Pishgooie et al., 2019). Consequently, nurse leaders may enhance employee contentment and care delivery by blending transformational and transactional styles of leadership. It is crucial for leaders to make the organization’s principles, goals, and purpose very obvious to everyone. They need to encourage workers by treating them with dignity, listening to their ideas, and believing in their potential.
Leaders in the nursing profession have a crucial role in helping their colleagues succeed in today’s demanding healthcare settings, fostering their development as nurses, and minimizing turnover rates. They are the individuals on whom nurses depend and who nurses seek assistance, and they are a unifying factor that may bring nurses together and encourage them to work together (Wei et al., 2020). Leaders who are capable of facing the challenge may lessen nurses’ stress by encouraging their participation in decision-making, providing them with opportunities for growth, demonstrating genuine and transformative leadership, and fostering a positive work atmosphere (Wei et al., 2020). The professional development of nurses and the prevention of burnout may both benefit from the leadership of nurses who serve as role models in these areas of importance.
Stress among Nurse Managers
The mental and physical health of nurse managers, as well as the well-being of their subordinates and the efficiency of their workplaces, suffer as a result of the high demands of management. Most of the stress that nurse managers feel comes from their enormous workloads, a shortage or absence of resources, and financial obligations (Labrague et al., 2018). In order to alleviate stress at work and prevent burnout and its repercussions, many people believe that it is crucial to provide social support and encourage workplace control (Labrague et al., 2018). Staffing, organizational resources, support programs, mentoring, and stress management coaching are all areas in which healthcare and nurse administrators may play a significant role in fostering a conducive environment for nurse managers’ everyday professional practice.
Medical-Surgical Nurses’ Job Satisfaction
Some of the elements that may help people appreciate their jobs more include having a supportive supervisor, a pleasant colleague group, and a reasonable workload and schedule. Pay and various types of bonuses might be motivating, but their effect can decrease quickly (Steele-Moses, 2021). Modern inpatients in medical and surgical wards are more critically ill than their predecessors were approximately a decade ago (Steele-Moses, 2021). Consequently, the severity of an individual’s condition should serve as the foundation for staffing strategies rather than nurse-to-patient ratios. Nurses’ morale and job security are impacted by managers’ actions and decisions. Nurses have high expectations of their supervisors, who they believe should be able to effectively run the unit where they work and keep them informed of any relevant developments.
In general, it can be stated that medical-surgical nurses’ motivation to remain employed in a medical-surgical unit is also heavily influenced by the unit’s culture. Satisfaction among nurses rises when they have a voice in unit decisions, connect and collaborate well with their coworkers, and are given a wide range of patients to care for (Steele-Moses, 2021). The research found that medical-surgical nurses valued aspects such as working alongside nurses who appreciated them, being able to participate in critical decisions, and being given opportunities for professional development in the workplace (Steele-Moses, 2021). Hence, this is why it is believed to be important for nurses to feel fulfilled in their careers.
Conclusion
To summarize, burnout in the healthcare industry has repercussions both for the individual practitioner and for, the patient and the organization as a whole. Various factors may contribute to patient safety being compromised, including inefficient collaboration and communication, dysfunctional organizational processes, and the emotional and physical strain placed on healthcare professionals. Burnout is a condition directly connected to a work engagement environment due to the stress that health and workers are always under on the job. This stress may lead to burnout. During their shifts, healthcare personnel is a subject to the impact of exhaustion, which is one of the regular dangers they confront. The personal ramifications that nurses experience as a result of emotional disorders and fatigue may lead to a variety of challenges, including those that involve interpersonal relationships.
Several different tactics are going to be offered as potential answers to the problem of preventing and combating burnout among nurses. The first technique to address nurse burnout is to improve the nursing work environment by developing and using a cultural change toolkit. This will allow for a more positive working atmosphere for nurses. Adopting a conceptualization of positive emotion skills treatments as a strategy is another approach that may be used to deal with the factors that contribute to burnout in nurses and emotional instability in the profession. The development of a social and individual work-led mindfulness-based intervention is one method that may be helpful for nurses working in a medical-surgical department.
The practice of mindfulness has the potential to cultivate a heightened awareness of one’s thoughts, feelings, and actions, as well as a changed sense of who one is and a more comprehensive appreciation for life. In addition, it is reasonable to advocate implementing a distinct mentoring program for internal communications for medical-surgical departments located inside hospitals. It is the responsibility of nursing leaders to assist their colleagues in achieving success in the challenging healthcare environments of today and to encourage their professional growth as nurses.
References
Adams, A., Hollingsworth, A., & Osman, A. (2019). The implementation of a cultural change toolkit to reduce nursing burnout and mitigate nurse turnover in the emergency department. Journal of Emergency Nursing, 45(4), 452-456. Web.
Arnetz, J. E., Goetz, C. M., Arnetz, B. B., & Arble, E. (2020). Nurse reports of stressful situations during the COVID-19 pandemic: Qualitative analysis of survey responses. International Journal of Environmental Research and Public Health, 17(21), 8126. Web.
Buckley, L., Berta, W., Cleverley, K., Medeiros, C., & Widger, K. (2020). What is known about pediatric nurse burnout: A scoping review. Human Resources for Health, 18(1), 1-23. Web.
Cheung, E. O., Hernandez, A., Herold, E., & Moskowitz, J. T. (2020). Positive emotion skills intervention to address burnout in critical care nurses. AACN Advanced Critical Care, 31(2), 167-178. Web.
Couser, G., Chesak, S., & Cutshall, S. (2020). Developing a course to promote self-care for nurses to address burnout. The Online Journal of Issues in Nursing, 25(3). Web.
Eweida, R. S., Rashwan, Z. I., Desoky, G. M., & Khonji, L. M. (2020). Mental strain and changes in psychological health hub among intern-nursing students at pediatric and medical-surgical units amid ambiance of COVID-19 pandemic: A comprehensive survey. Nurse Education in Practice, 49, 102915. Web.
Falatah, R. (2021). The impact of the coronavirus disease (COVID-19) pandemic on nurses’ turnover intention: An integrative review. Nursing Reports, 11(4), 787-810. Web.
Garcia, C. L., Abreu, L. C., Ramos, J., Castro, C., Smiderle, F., Santos, J., & Bezerra, I. (2019). Influence of burnout on patient safety: Systematic review and meta-analysis. Medicina, 55(9), 553. Web.
Jun, J., Ojemeni, M. M., Kalamani, R., Tong, J., & Crecelius, M. L. (2021). Relationship between nurse burnout, patient and organizational outcomes: Systematic review. International Journal of Nursing Studies, 119, 103933. Web.
Kelly, L. A., Gee, P. M., & Butler, R. J. (2021). Impact of nurse burnout on organizational and position turnover. Nursing Outlook, 69(1), 96-102. Web.
Krofft, K., & Stuart, W. (2021). Implementing a mentorship program for new nurses during a pandemic. Nursing Administration Quarterly, 45(2), 152-158. Web.
Labrague, L. J., McEnroe‐Petitte, D. M., Leocadio, M. C., Van Bogaert, P., & Cummings, G. G. (2018). Stress and ways of coping among nurse managers: An integrative review. Journal of Clinical Nursing, 27(7-8), 1346-1359. Web.
Phillips, C. (2020). Relationships between workload perception, burnout, and intent to leave among medical–surgical nurses. JBI Evidence Implementation, 18(2), 265-273. Web.
Pishgooie, A. H., Atashzadeh‐Shoorideh, F., Falcó‐Pegueroles, A., & Lotfi, Z. (2019). Correlation between nursing managers’ leadership styles and nurses’ job stress and anticipated turnover. Journal of Nursing Management, 27(3), 527-534. Web.
Schlak, A. E., Rosa, W. E., Rushton, C. H., Poghosyan, L., Root, M. C., & McHugh, M. D. (2022). An expanded institutional- and national-level blueprint to address nurse burnout and moral suffering amid the evolving pandemic. Nursing Management, 53(1), 16. Web.
Sexton, B., Levine, L. K., & Flores, D. (2021). An analysis of nurse burnout in the emergency department. Journal of Business and Behavioral Sciences, 33(1), 94-108. Web.
Shah, M. K., Gandrakota, N., Cimiotti, J. P., Ghose, N., Moore, M., & Ali, M. K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA Network Open, 4(2), e2036469-e2036469. Web.
Steele-Moses, S. K. (2021). Predicting medical-surgical nurses’ work satisfaction and intent to stay. Nursing Management, 52(8), 16-25. Web.
Wampole, D. M., & Bressi, S. (2020). Exploring a social work lead mindfulness-based intervention to address burnout among inpatient psychiatric nurses: A pilot study. Social Work in Health Care, 59(8), 615-630. Web.
Wei, H., King, A., Jiang, Y., Sewell, K. A., & Lake, D. M. (2020). The impact of nurse leadership styles on nurse burnout: A systematic literature review. Nurse Leader, 18(5), 439-450. Web.
Appendices