Similarities and Differences between the Transtheoretical Model (TTM) and the Health Belief Model (HBM)
Similarities
Both HBM and TTM strive to predict how people adopt preventive health practices to protect themselves from diseases (Seals, 2007). Both models also focus on increasing people’s awareness about health issues as an instrument for encouraging preventive health (Atak, 2008).
Differences
HBM mostly focuses on investigating cognitive issues that influence human behavior (Noroozi, Jomand, & Tahmasebi, 2011). It does not focus on explaining the emotional issues that affect human behavior. Comparatively, TTM focuses on the behavioral aspects of human actions. Particularly, it strives to understand the attitudinal aspects of health behavior that would influence behavior change (Humiston et al., 2011).
Application of TTM to the Health Issue
TTM works by demonstrating the need to apply specific behavioral change strategies at the right time (Glanz, Rimer, & Viswanath, 2015). The theory applies to the chosen health issue (breast cancer) because it outlines the distinctive stages that health workers could introduce behavior change strategies. The stages are pre-contemplation, relapse, contemplation, relapse risk, action, and maintenance (Glanz et al., 2015). By knowing these stages, it is easy to identify the right type of behavioral change strategy to use for each type of person involved. In other words, public health workers are saved from the problem of “guessing” the best intervention to use for a specific person. The stages of the change model appear below
Application of Health Belief Model to the Chosen Action
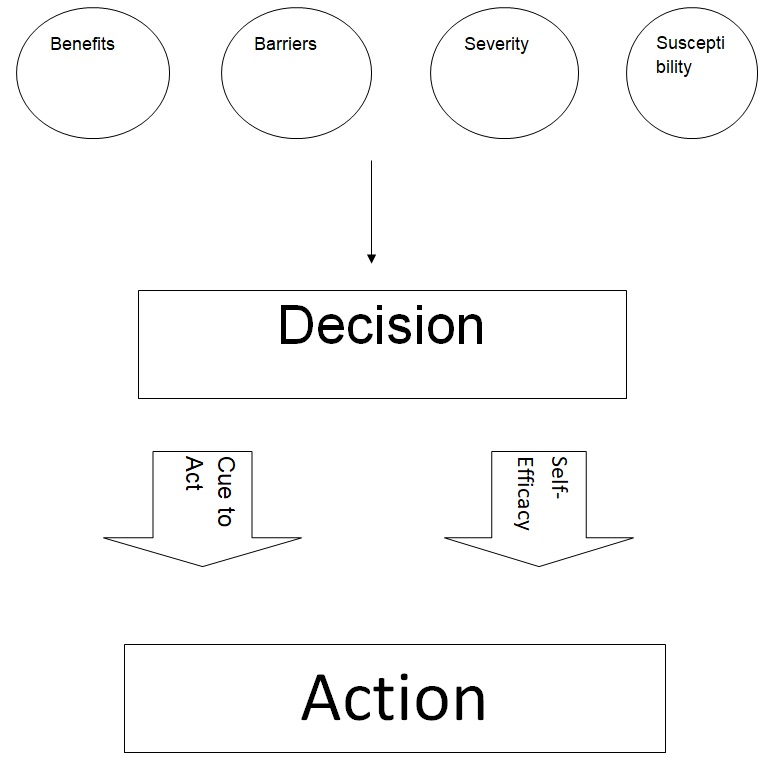
The health belief model works by investigating the influence of four perception factors that strive to predict human health behaviors. These four factors are benefits, barriers, severity, and susceptibility. In the context of the assigned study, these four factors would define the perception of Iranian women regarding self-breast examination (National Cancer Institute, Rimer, & Glanz, 2005). Using this perception, they would decide the health issue. The decision would prompt them to take action, or not. The cue to act, or self-efficacy, would influence this action. The diagram below provides a summary of how the HBM would apply to the chosen health issue.
Which Model is most appropriate?
I believe the HBM model is the most appropriate theory to use for the selected research issue because it considers the social context that influences behavior change. The social context of behavior change is pertinent to our understanding of the health issue because Iran is a religious society and women’s health is subject to specific social and religious norms. TTM fails to recognize the social context, which underpins change (Glanz et al., 2015). The theory also assumes that people’s decision-making process is often logical and coherent. However, this is false, especially for a country like Iran where women shy away from engaging in healthy behaviors that contravene social, patriarchal, and religious norms (Noroozi et al., 2011).
Conclusion and Suggestion
Although TTM and HBM are similar in the sense that both of them try to predict health behaviors by analyzing individual factors that would influence the same, TTM outlines a systematic process that would explain people’s path towards wellness and wellbeing. Comparatively, HBM strives to outline different factors that would contribute towards explaining people’s health behaviors. TTM is useful in instances when health workers have ample time to study, or guide, a specific population to attain a predetermined health objective. HBM could be useful in situations where there is not ample time to do so. However, considering both theories have their distinct advantages and disadvantages, I would suggest that health workers use them concurrently.
References
Atak, N. (2008). A transtheoretical review on smoking cessation. International Quarterly of Community Health Education, 28(2), 165–175.
Glanz, K., Rimer, B. K., & Viswanath, K. (Eds.). (2015). Health behavior: Theory, research, and practice (5th ed.). San Francisco, CA: Jossey-Bass.
Humiston, S. G., Marcuse, E. K., Zhao, Z., Dorell, C. G., Howes, C., & Hibbs, B. (2011). Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the health belief model. Public Health Reports, 126(Suppl. 2), 135–146.
National Cancer Institute, Rimer, B. K., & Glanz, K. A. (2005). Theory at a glance: A guide for health promotion practice (2nd ed.). Washington, DC: U.S. Department of Health and Human Services, National Institutes of Health.
Noroozi, A., Jomand, T., & Tahmasebi, R. (2011). Determinants of breast self-examination performance among Iranian women: An application of the health belief model. Journal of Cancer Education, 26(2), 365–374.
Seals, J. G. (2007). Integrating the transtheoretical model into the management of overweight and obese adults. Journal of the American Academy of Nurse Practitioners, 19(2), 63–71.