Background
Research on tuberculosis has a long history, but science does not allow humanity to stop its spread, and it still has a global incidence. Tuberculosis is a chronic infectious disease caused by the bacteria M. tuberculosis, initially discovered at the end of the 19th century by Robert Koch (Churchyard et al., 2017). Tuberculosis remained an incurable disease that led to death for decades after the bacteria was discovered. Healthcare professionals did not completely understand the risks connected with this disease and its transmission mechanisms. In the 1920s, healthcare workers acknowledged that they were at risk while communicating with patients diagnosed with tuberculosis (Churchyard et al., 2017). A decade after it, Wells described the transmission of the bacteria and the scheme of contamination, which made the situation clearer concerning contact with patients. Only in the 1970s did the researchers describe the risks of all people who live in one household with a person with tuberculosis (Churchyard et al., 2017). The critical detail is that the investigations did not help epidemiologists stop the spread of tuberculosis, and nowadays, it is possible to talk about the pandemic of this infection.
Transmission
Tuberculosis is a highly contagious disease, and it has airborne transmission. Due to its rapid spread, it remains a global problem nowadays, and humanity cannot cope with it. According to the World Health Organization estimates, almost 10,5 million are diagnosed with tuberculosis annually (Churchyard et al., 2017). It is possible to describe the main reasons for tuberculosis transmission in several steps. A person who has tuberculosis generates particles that are already infectious and spreads them in the air while coughing or speaking; other individuals inhale these infected particles and may also become infected with tuberculosis. The critical detail is that some people have higher contamination risks due to low immunity affected by various issues. Among them are smoking and diagnoses like AIDS or HIV that negatively affect human health (Churchyard et al., 2017). In general, tuberculosis transmission is typical for airborne contagious diseases, making it predictable and understandable for scholars, but it does not help eliminate the illness.
Morbidity
Prevalence and Incidence
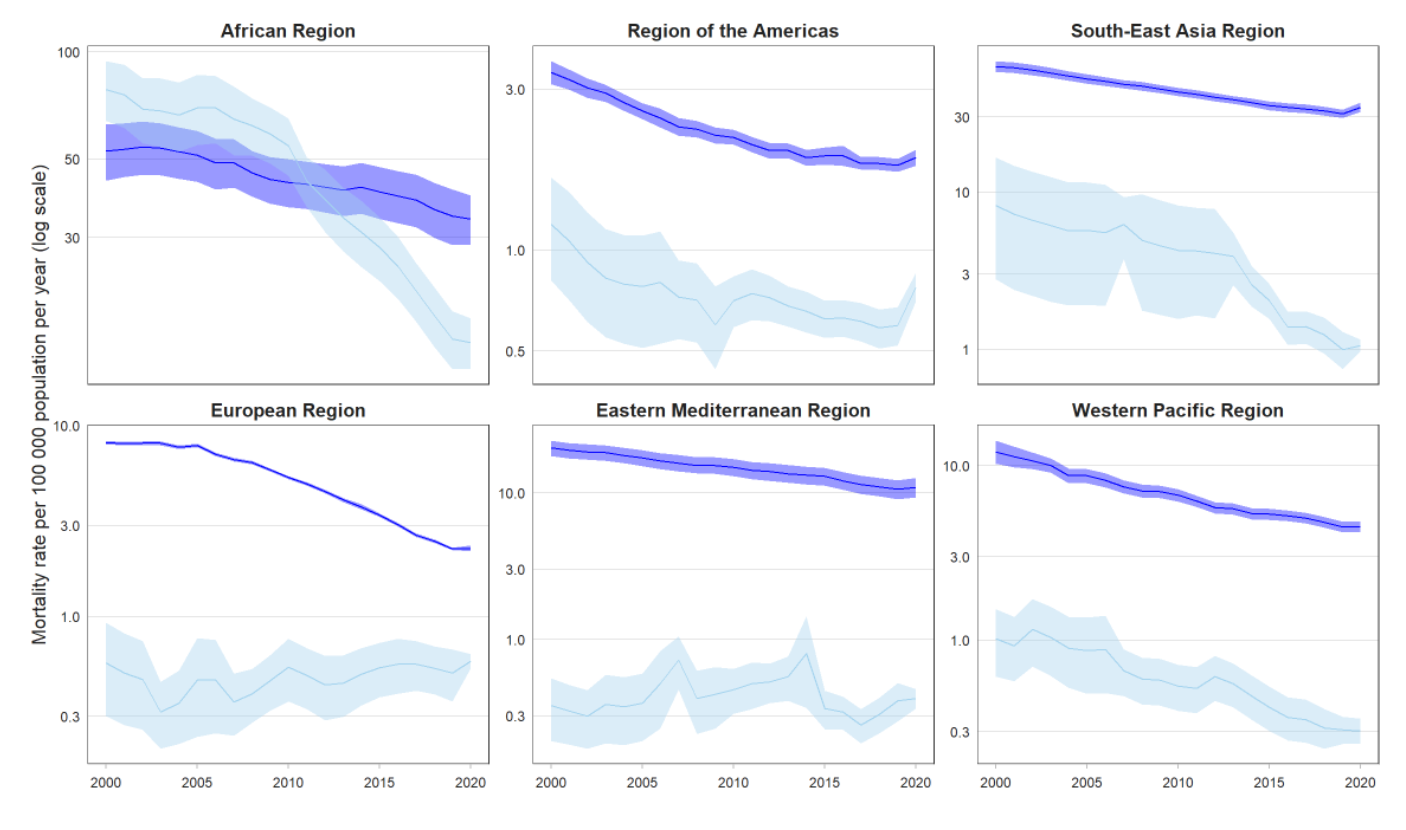
Due to different factors, the prevalence of the disease and morbidity rates vary across countries and nations. For instance, some ethnic groups show higher mortality from tuberculosis than others, including the Native American population in the United States. More than 80% of all deaths from tuberculosis in the United States happen among ethnic minorities (Churchyard et al., 2017). This information shows that diverse populations are affected by tuberculosis differently, which is essential in the epidemiological analysis of the disease. The World Health Organization provides the following graphs that illustrate the incidence and the prevalence of tuberculosis across regions (Figure 1):
Mortality Rates and Proportions
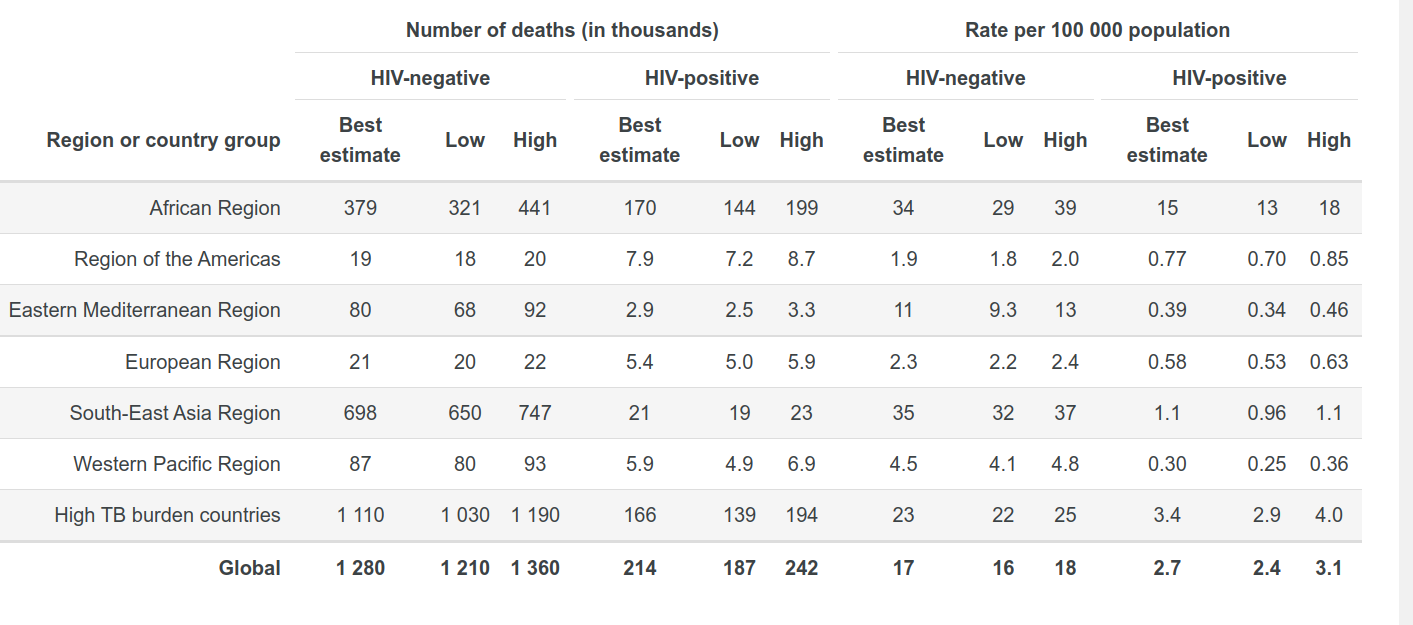
In general, mortality rates of tuberculosis decreased significantly after the use of antibiotics in its treatment, timely diagnosis, and vaccination that controls the spread of the infection (Churchyard et al., 2017). At the same time, the results concerning mortality rates and effectiveness of treatment are different in various states due to the level of public healthcare. It is possible to illustrate the tuberculosis mortality rates across countries using the following table 1 with the information provided by the World Health Organization:
Pneumonia is the main sign of lung infection, but pneumonia caused by the bacteria M. tuberculosis has a distinctive development. While typical pneumonia has adverse effects on the airways, tuberculosis destroys the lungs, and its pneumonia is characterized by typical granuloma or hallmarks (Guinn & Rubin, 2017). It is possible to descry the inflammatory process in the following way:
“… several features are moderately distinctive for TB—an area of central cell death, lipid-filled “foamy” macrophages and “giant cells,” multinucleate syncytia formed from fused macrophages. As necrosis proceeds, the boundaries of the granuloma can erode into airways, allowing their contents to be aerosolized ” (Guinn & Rubin, 2017).
These lines show that scientists thoroughly research the inflammation process and its transmission. However, tuberculosis is a severe disease that destroys the human lungs gradually if the ill person does not receive timely medical help and treatment. It often endangers the health state of most people in the community, which makes the individual with tuberculosis the reason of the bacteria spreading.
The duration and severity of the illness depend on various factors, leading to differences in the course of the disease. For instance, the bacteria’s characteristics and the host’s immunity determine the health outcomes for a particular individual. Those who have smear-positive pulmonary tuberculosis are significantly more infectious than individuals with other types of tuberculosis (Churchyard et al., 2017). This type of bacteria means that the household members where the person with tuberculosis leaves have higher risks of contamination. Smear-negative types of tuberculosis, in its turn, have milder symptoms of the disease and are less dangerous for other individuals (Churchyard et al., 2017). At the same time, it is challenging for scientists to determine smear-negative bacteria of tuberculosis due to its low sensitivity to the existing methods of diagnostics (Churchyard et al., 2017). It shows that the characteristics of the M.tuberculosis bacteria are critical in analyzing its transmission and the severity of the illness.
The critical detail concerning the transmission of tuberculosis is the duration and the frequency of exposure to the infection. It is unlikely that the person will become infected with tuberculosis if the contact is short. Though, individuals who live in one household, work together in one office, or communicate regularly have higher chances of becoming infected with tuberculosis if they are ill (Guinn & Rubin, 2017). Therefore, the transmission of tuberculosis is predominantly airborne, but people need close and frequent contact for contamination.
Outbreaks
Tuberculosis is among the concerns of global healthcare nowadays, which means that humans cannot cope with the outbreaks of the disease. The World Health Organization makes the prognosis that the number of people infected with tuberculosis will decrease by 10% annually in 2025, but in 2017 this rate was only 1.5% (Churchyard et al., 2017). At the same time, a 10% decline in the incidents of tuberculosis is possible to achieve, and this rate was stable in the 1950s – 1960s in the countries of Western Europe. A high level of treatment and infection control combined with the public access to healthcare for all socioeconomic groups made these results possible (Churchyard et al., 2017). In all cases, the international healthcare community makes everything possible to achieve a decline in tuberculosis outbreaks, but it is impossible to eliminate the disease in all corners of the world.
It is essential to remember that tuberculosis is a widespread and common illness in most countries. As a result, people are not afraid of this infection because it is not a new concern. Individuals think that tuberculosis is the illness of the poor who live in difficult conditions, which gives them the illusion of immunity against tuberculosis (Guinn & Rubin, 2017). In reality, people of all social and economic backgrounds can become infected with tuberculosis. Sometimes, it is challenging to diagnose it because people do not think they can have this illness (Churchyard et al., 2017). According to the World Health Organization estimates, the number of outbreaks of tuberculosis is more than 8 million cases annually (Guinn & Rubin, 2017). It is vital to remember that tuberculosis has killed more people than HIV throughout history (Guinn & Rubin, 2017). For this reason, it is critical to pay much attention to the outbreaks of tuberculosis because it remains a danger to public health worldwide.
Surveillance
The surveillance over tuberculosis shows that the infection has severe outcomes for human health, especially when the infected person is in the risk group. The case study and experiment conducted by Di Gennaro et al. (2022) in an Italian hospital shows that demographic characteristics are essential in predicting the outcomes of the infections. For instance, there was a critical difference between the length of hospital stay of the elderly and the young patients diagnosed with tuberculosis. Younger patients tend to stay two times less than older patients (43 days on average of 24 days reciprocally) (Di Gennaro et al., 2022). This data might seem strange from an objective point of view because younger people supposedly have a better immune system, which protects them from tuberculosis. In reality, their immune response to tuberculosis is more active compared to the elderly populations, but it requires more time (Di Gennaro et al., 2022). Therefore, the length of the hospital stay is a biased factor in disease surveillance.
Another point that Di Gennaro et al. mention in the case study is connected with social determinants of patients with tuberculosis. The number of immigrants and homeless people among them is significantly higher than those without economic and social concerns (Di Gennaro et al., 2022). The researchers describe this situation with the social and economic context of tuberculosis in the following lines:
“The pharmacological approach alone seems insufficient to treat and cure a disease whose etiopathogenesis is not only due to the Mycobacterium tuberculosis but also to the poverty or the social fragility. Our data suggest that young foreigners, the homeless, and people with low social and economic status are at higher risk of an unfavorable outcome in low incidence TB countries” (Di Gennaro et al., 2022, p. 1).”
This data illustrates the hypothesis that the conditions of life and the access to public health are vital elements in the surveillance of tuberculosis.
There are limitations to the treatment of this infection in developing countries. The case study by Kazibwe et al. (2022) focuses on tuberculosis treatment in Uganda, where many people do not have equal access to isoniazid preventive therapy for tuberculosis. Even though this treatment method effectively reduces the level of contamination in the region, it is challenging for the public health system in developing countries to cover its expenses. As a result, healthcare professionals often choose between patients with tuberculosis who is more eligible for treatment and prefer people with HIV because they have higher health risks (Kazibwe et al., 2022). This case study reflects that unfavorable outcomes of tuberculosis are connected with social and economic factors connected with the spread of the infection.
Screening
Tuberculosis is a latent infection that does not manifest itself for a comparatively long time. As a result, the person does not know that they are infected for months before the first symptoms appear. Latency of tuberculosis leads to its active transmission and the severity of health outcomes for the infected individual who does not receive medical help in the first stages of the disease (Guinn & Rubin, 2017). Therefore, screening and diagnosing tuberculosis remains one of the priorities for healthcare. Despite all existing methods of screening, the results are still far from ideal due to the character of the infection and problems with its timely diagnostic when patients do not know that they are ill.
Blood tests and skin tests allow healthcare professionals to understand whether the individual is infected with tuberculosis. Moreover, it reflects the progress of the disease, which allows physicians to control the patient’s health state (Churchyard et al., 2017). One innovative test that determines M.tuberculosis bacteria is the Xpert MTB/RIF (Churchyard et al., 2017). It changed the effectiveness of the diagnostics due to its increased sensitivity to the bacteria compared to the old methods. At the same time, the Xpert MTB/RIF implementation did not allow healthcare professionals to decrease the mortality rate from tuberculosis because it depends on public health in general (Churchyard et al., 2017). Therefore, screening is essential in minimizing the risks of tuberculosis, but at the same time, it does not solve the problems connected with its spread.
Risk Estimation
As mentioned, people with problems with immunity and those who have close contact with infected individuals have higher risks of contamination. It is typical for the respiratory infections that have the airborne type of spreading. The case study results show that developing countries with financial problems in public healthcare prioritize patients with HIV in tuberculosis treatment because they have higher morbidity risks (Kazibwe et al., 2022). Therefore, the health status of a particular person is critical in the risk estimation of the patient.
The COVID-19 infection increases the mortality risks of people diagnosed with tuberculosis. The case study conducted in Turkey in 2020 showed that COVID-19 and tuberculosis had become overlapping respiratory infections. Patients with both diagnoses die from pulmonary tuberculosis or cannot cope with their illness for a long time. According to the investigation, of 148,067 cases of tuberculosis and COVID-19, 4096 people died (Can Sarınoğlu et al., 2020). This information shows that overlapping respiratory infections harm human health and increase the individual’s risk of becoming ill with tuberculosis.
Causation and Inference
Scholars have diverse opinions concerning the causes of the tuberculosis spread. According to the case study conducted by Chen et al., environmental factors increase the spread of tuberculosis. For instance, prolonged exposure to air pollution leads to higher risks of lung infections and disrupts the secretion and the synthesis of inflammatory cytokines (Chen et al., 2022). Therefore, air pollution aggravates tuberculosis symptoms and contributes to its spreading among populations.
At the same time, tuberculosis is a chronic disease caused by the contamination with the bacteria M.tuberculosis. Close and long-term contact with the ill person is critical in spreading the disease. Therefore, the pollution of the environment can cause problems with the respiratory system and weaken the person’s immunity, but contamination is impossible without contact with the infection. It illustrates the hypothesis that timely immunization, diagnostics, and treatment of people with tuberculosis are critical in controlling the spread of the disease.
References
Can Sarınoğlu, R., Sili, U., Eryuksel, E., Olgun, Yildizeli, S., Cimsit, C., Karahasan, Y. A. (2020). Tuberculosis and COVID-19: An overlapping situation during pandemic. J Infect Dev Ctries 14(7), 721-725.
Chen, Y.P., Liu, L.F., Che, Y., Huang, J., Li, G.X., Sang, G.X., Xuan, Z.Q., He, T.F. (2022). Modeling and predicting pulmonary tuberculosis incidence and its association with air pollution and meteorological factors using an ARIMAX model: An ecological study in Ningbo of China. International Journal of Environmental Research and Public Health 19(9), 1-11.
Churchyard, G., Kim, P., N., Shah, S., Rustomjee, R., Gandhi, N., Mathema, B., Dowdy, D., Kasmar, A., Cardenas, V. (2017). What we know about tuberculosis transmission: An overview. The Journal of Infectious Diseases 216(6), 629-635.
Di Gennaro, F., Lattanzio, R., Guido, G., Ricciardi, A., Novara, R., Patti, G., … Saracino, A. (2022). Predictors for Pulmonary Tuberculosis Outcome and Adverse Events in an Italian Referral Hospital: A Nine-Year Retrospective Study (2013–2021). Annals of Global Health, 88(1), 1-12.
Guinn, K. M. & Rubin, E. J. (2017). Tuberculosis: Just the FAQs. Department of Immunology and Infectious Diseases, 8(6), 1-14.
Kazibwe, A., Oryokot, B., Mugenyi, L., Kagimu, D., Oluka, A. I., Kato, D., Ouma, S., Tayebwakushaba, E., Odoi, C., Kakumba K., Opito, R., Mafabi, C. G., Ochwo, M., Nkabala, R., Tusiimire, W., Kateeb, A., Alinga, S. B., Miya, Y., Etukoit, M. B., Biraro, I. A., Kirenga, B. (2022). Incidence of tuberculosis among PLHIV on antiretroviral therapy who initiated isoniazid preventive therapy: A multi-center retrospective cohort study. PLoS One 16(5), 1-13.
World Health Organization. (2021). Global tuberculosis report 2021.