Introduction
Urinary tract infection (UTI) is a very common adverse event in long-term care (LTC) facilities (Genao & Buhr, 2012). It is also often overdiagnosed and overtreated, especially in the elderly population, which is not beneficial for the patients because of unnecessary antibiotics exposure (Grigoryan, Trautner, & Gupta, 2014; Lim, Whitehurst, Usoro, & Ng, 2014). The present article intends to visualize and review the workflow of UTI management in LTC with the aim of determining the potential for improvement. To this end, a flowchart will be used due to the ability of this tool to visually demonstrate the steps that are involved in the workflow (U.S. Department of Health & Human Services [DHHS], n.d.). The key actions and actors will be determined, and a conclusion will be made about possible flaws, improvements, and the significance of workflow analysis.
UTI Management Workflow Process
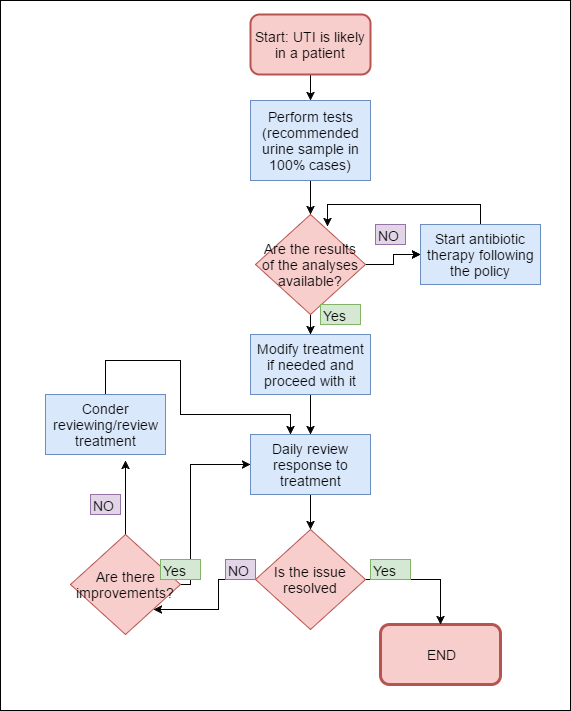
The following flowchart considers UTI management processes.
Explanation of the Workflow Process
The determination of the likelihood of UTI requires a separate flowchart because it involves assessing multiple symptoms and ruling out other infections (Genao & Buhr, 2012; Lim et al., 2014). As a result, the present flowchart of the process begins with the likelihood of UTI already established. When the symptoms are suggestive of UTI and not another infection, the following steps are of importance.
The first step involves performing the tests which should enable the determination of appropriate treatment; the information that is necessary for its element of the flow is provided when the likelihood of UTI is determined. It is strongly recommended that a urine sample is obtained and sent for analysis (Lim et al., 2014), but other tests may be in order, especially in case the urine sample does not provide sufficient confirmation of the presence of UTI (Genao & Buhr, 2012).
The samples are obtained and sent for analysis by the nursing staff. Technology is unlikely to be used during urine collection, but there exist guidelines on techniques, as well as specific equipment, that should be employed to ensure the collection of a non-contaminated sample. For example, in older adults with physical or cognitive constraints, catheterization, and clean catch technique can be used (Latour et al., 2013).
The following step involves defining and using appropriate therapy. Before the results of the analyses are provided, standard UTI treatment policy guides the decision, but after the results are available, it should be modified if necessary (Lim et al., 2014). Thus, the required information for the step includes the results of the analysis; the guidelines that define how the step is executed are the standard UTI treatment policies (Genao & Buhr, 2012). The treatment is administered by nurses; depending on the specifics of treatment, special technology, equipment, and techniques may be necessary (for example, in the case of intravenous medication use) (Wagenlehner, Umeh, Steenbergen, Yuan, & Darouiche, 2015).
After the treatment is provided, nurses are supposed to review the response to treatment and define if there is an improvement on a daily basis. In particular, the changes in symptoms should be monitored with the help of appropriate technology and techniques (for example, digital thermometers to measure body temperature or an examination aimed at determining the changes in swelling). Thus, this step requires the consistent collection of information; the process is necessary to ensure the patient’s safety and the appropriateness of treatment, and it is required by the institution’s guidelines.
If no improvement is found, a review of the treatment should be considered. This step involves nurse consulting with other specialists; it requires the information provided by the previous step, and it is guided by the institution’s policies. No technology is expected to be used in the process (unless clinical decision support is deemed necessary) since all the information is provided by the previous step.
Metrics used for Workflow Evaluation
Several metrics should be used for the assessment of the workflow of UTI management. In particular, the percentage of correct diagnoses is important. Apart from that, the instances of treatment revision and the presence of complications can inform the understanding of the use of appropriate tests and antibiotics. Moreover, the time that is spent between the stages (in particular, between the determination of UTI and the collection of samples) is significant from the point of view of the effectiveness of the workflow and is important for the determination of correct treatment early in the workflow (Lim et al., 2014).
The metrics can be regarded as effective since they target the quality and safety concerns and operationalize the factors of interest. Their only constraint is that they require meticulous and meaningful documentation of the process in order to be effective. However, this factor can also be regarded as an advantage since documentation is critical for the care as well as the improvement of the workflow (Hammel-Jones, McGonigle, & Mastrian, 2015)
Areas for Improvement
While not revealing particular flaws, the flowchart demonstrates that the time between the determination of the likelihood of UTI and the collection of the required samples may be crucial for defining appropriate treatment. While the nurses cannot affect the time needed for the analysis, they can affect the time before the samples are collected, which calls for the improvement of this indicator. According to Lim et al. (2014), educational measures aimed at the staff, as well as improved feedback and communication between the nurses, their leaders, and managers, as well as doctors, are likely to improve the situation and promote fast action in the case of UTI likelihood.
Conclusion
The present paper considers the workflow of UTI management in LTC. The workflow includes obtaining the results of tests, customizing treatment, and monitoring it. The key actors of the process are nurses, but other specialists are also involved. The metrics include tracking the correct and incorrect diagnoses and treatment decisions and time-related factors. All these metrics should help to minimize the issues of over-diagnosing and overtreatment, and they also indicate potential areas for improvement, especially in terms of time. The latter can be improved through educational interventions.
As suggested by the present example, the awareness of the flow of activity is important because it helps to reveal the key stages and actors of the process, informing its analysis. The analysis, on the other hand, allows revealing the inefficiencies in the workflow, which offers an opportunity for revision and improvement (DHHS, n.d.). According to Hammel-Jones et al. (2015), the analysis of the workflow is not optional; rather, it is a requirement for continuous improvement and the customization of solutions to fit every particular institution (p. 242). It is necessary for efficient care, and as more advanced, technology-enabled methods of workflow modeling are created (Huser, Rasmussen, Oberg, & Starren, 2011), more opportunities for the improvement of processes become available.
References
Genao, L., & Buhr, G. T. (2012). Urinary tract infections in older adults residing in long-term care facilities. The Annals of Long-Term Care: The Official Journal of the American Medical Directors Association, 20(4), 33-38.
Grigoryan, L., Trautner, B., & Gupta, K. (2014). Diagnosis and Management of Urinary Tract Infections in the Outpatient Setting. JAMA, 312(16), 1677.
Hammel-Jones, D., McGonigle, D., & Mastrian, K. (2015). Nursing informatics: Improving workflow and meaningful use. In D. McGonigle & K.G. Mastrian (Eds.), Nursing informatics and the foundation of knowledge (pp. 229-244). Burlington, MA: Jones and Bartlett Learning.
Huser, V., Rasmussen, L. V., Oberg, R., & Starren, J. B. (2011). Implementation of workflow engine technology to deliver basic clinical decision support functionality. BMC Medical Research Methodology, 11(1), 43–61.
Latour, K., Plüddemann, A., Thompson, M., Catry, B., Price, C., Heneghan, C., & Buntinx, F. (2013). Diagnostic technology: alternative sampling methods for collection of urine specimens in older adults. Family Medicine and Community Health, 1(2), 43-49.
Lim, V., Whitehurst, T., Usoro, E., & Ng, S. (2014). Management of urinary tract infections in elderly patients: Strategies for improvement. BMJ Quality Improvement Reports, 3(1), 1-3.
U.S. Department of Health & Human Services. (n.d.). Workflow assessment for health IT toolkit.
Wagenlehner, F., Umeh, O., Steenbergen, J., Yuan, G., & Darouiche, R. (2015). Ceftolozane-tazobactam compared with levofloxacin in the treatment of complicated urinary-tract infections, including pyelonephritis: a randomised, double-blind, phase 3 trial (ASPECT-cUTI). The Lancet, 385(9981), 1949-1956.