Introduction
The occurrence of obesity is growing around the globe at a disturbing rate in both developed as well as developing countries (World Health Organization, 2000). In the European countries, the prevalence of obesity ranges between 10 and 20% in men and between 15 and 25% in women, while in the US the prevalence of adult obesity currently stands at 28% among men and 34% among women. Overweight is the sixth most significant risk factor that causes the global health burden.
Obesity increases the risks of “type 2 diabetes, hypertension, cardiovascular disease, dyslipidemia, arthritis, and several cancers” (Haslam and James, 2005, p.1199) and is believed to lessen the average life expectancy. A negative energy balance caused by the management of obesity normally creates a decline in the fat stores and a suitable conservation of lean body mass. A preferential lessening of abdominal fat, a decrease in obesity-related health risks, an enhancement in comorbidity and in quality of life, and a fall in mortality rate are some of the most vital goals of obesity treatment (Anderson, Konz, Frederich and Wood, 2001). An effective treatment programs for obese patients ought to have a significant impact on the utilization of medical resources and on the costs of health care.
Issues/problems
Physicians and other health care providers encounter a great problem in helping obese patients not only to normalize their weight but also to attain weight loss maintenance. Indeed, weight regain is one of the most common problems that obese patients face during their treatment. Ross (2009) argues that, “Most patients regain about 30% of the weight lost in the year following treatment and typically return to their baseline weight in 3-5 years,” (p.997).
A number of factors such as the type of support offered to the patients, the types of diets followed by the patients and the type and intensity of physical activity performed by the patients affect the ability (or lack thereof) of the patients to maintain the weight loss. It is however important for health care providers to individually tailor the treatment of the obese patients according to their “age, sex, degree of obesity, individual health risks, metabolic and psycho-behavioral characteristics, and outcome of previous weight loss attempts,” (Hainer, Toplak and Mitrakou, 2008, p.273).
All in all, the goals set in the obesity treatment programs should be realistic because unrealistic goals of weight loss often lead to a failure in weight loss maintenance. In order to reduce weight to a normal level, a low-energy diet, physical exercises and healthcare support programs should be implemented for the obese patients. A normal weight is measured by the body mass index (BMI) which takes into account the height and weight of an individual. Normally a person is said to be obese if he/she has a BMI of 30 or more.
Low energy diet
A low-energy diet commended for the treatment of obesity should be low fat (<30%), high carbohydrate (~55% of daily energy intake), high protein (up to 25% of daily energy intake), and high fiber (25 g/day) (Pirozzo, Summerbell, Cameron and Glasziou, 2003). A moderate decrease in energy intake (-2.5 MJ/day) could lead to a sluggish (~2.5 kg/month) and constant weight loss. So far, many research studies provide evidence that suggest that the total energy intake in diets is a key determining factor of the ability of obese patients to lose weight. It should be noted that diets that provide <5 MJ/day may create shortages of numerous micronutrients, which could have unpleasant effects on nutritional status as well as on the weight management result (Heymsfield, van Mierlo, van der Knaap, Heo and Frier, 2003).
Physical activity
Physical activity should be an essential component of an all-inclusive obesity management program and should be individually customized according to the extent of obesity, age, and existence of comorbidities in each patient. Physical activity contributes to “a higher energy spending and fat loss and also protects patients from losing lean body mass, enhances cardiorespiratory fitness, minimizes obesity-related cardio-metabolic health risks, and stirs feelings of general well-being,” (Phalan, Wyatt, Hill and Wing, 2006, p.712).
Aerobic physical exercise contributes to enhancement in oxygen flow to muscle, which in turn encourages an increased use of excess fat stores rather than the scarce glycogen stores (Wing and Hill, 2001). The recommended intensity of physical activity is a moderate activity done for 30 minutes, 5 days a week. In a month, such an activity can lead to a loss of 0.5 kg of weight. Patients ought to be familiar with the rational goals regarding the anticipated exercise-induced weight loss in addition to the positive effects of exercise on cardio-metabolic risks. To maximize weight loss, the intensity of physical activity should be doubled to 60 minutes for 5 days a week.
Obesity normally results from a habitual sedentary lifestyle. Thus, patients should be encouraged to undertake activities such as walking, cycling, and stair climbing (Wing, 1999). The use of physical activity to manage weight is positively associated with the level of education and, on the other hand, negatively associated with the prevalence of serious comorbidities, age and extent of overweight. Patients who suffer from severe arthritis and other mobility problems should exercise in heated water. Patients should avoid engaging in “vigorous physical activity that can lead to joints overloading, such as jumping” (Phalan, Wyatt, Hill and Wing, 2006, p.713).
The protection of lean body mass and minimization of health risks can be done through strength exercise modalities although such exercises do not enhance lipid oxidation. All sorts of regular physical activities symbolize a significant aspect that leads to lasting maintenance of weight loss.
Health care support programs
Besides diets and exercises, weight management in obese patients can be achieved through the receipt of health care support services. Such services can be offered by physicians, nurses, nutritionists, and exercise specialists among others. Research shows that obese patients who are enrolled in a nurse-supported group and who engage in regular contacts with their nurses (both face-to-face and via the telephone) and who are engaged in self-weighing of weight are more likely than others to succeed in maintaining their weight loss (Dale, McAuley and Taylor, 2009). This is because the constant contact with nurses enables the nurses to monitor the progress of the patients on a regular basis than would be possible if the contact was lacking or minimal.
The major challenge of implementing nurse-coordinated support programs lies in the shortage of nurses who may be already overworked. It is therefore important to include other specialists such as nutritionists and exercise exerts to assist the nurse. The advantage of such an inclusion is that the specialists are knowledgeable and skilled in their areas of expertise and are therefore most likely to provide the best possible care to the patients. In addition, such specialists “have the relevant training, are no more expensive than nurses, and would be enthusiastic supporters of their nursing colleagues,” (Ross, 2009, p.998).
Purpose of the database
The purpose of the database is to:
- Determine the effectiveness of a low-energy diet, physical activity and a nurse-coordinate support program in losing weight.
- Determine the effectiveness of a low-energy diet, physical activity and a nurse-coordinated support program in preventing weight regain among obese patients: Six months after the onset of the program; one year after the onset of the program; three years after the onset of the program; and five years after the onset of the program.
The database will therefore track the progress of the obese patients for five years after they begin their weight management program.
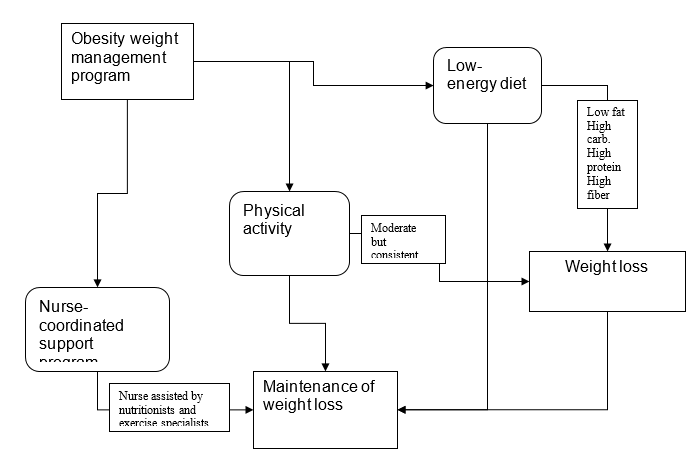
Data flow diagram: weight loss and management program
Data dictionary
From the above issue statement and data flow diagram, five tables will be created namely: Demographics, Low energy diet, Physical activity, Nurse-coordinated program, and Body mass index. The tables will have twenty-one fields in total and fifty records in total.
Reference List
Anderson, J.W., Konz, E.C., Frederich, R.C., & Wood, C.L. (2001). Long-term weight-loss maintenance: a meta-analysis of US studies. American Journal of Clinical Nutrition 74, 579-584.
Dale, K.S., McAuley, K.A., & Taylor, R.W. (2009). Determining optimal approaches for weight maintenance: a randomized controlled trial. CMAJ 180, 1015-20.
Hainer, V., Toplak, H., & Mitrakou, A. (2008). Treatment modalities of obesity: What fits whom? Diabetes Care 31, 269-276.
Haslam, D.W., & James, W.P.T. (2005). Obesity. Lancet 366, 1197-1209.
Heymsfield, S.B., van Mierlo, C.A., van der Knaap, H.C., Heo, M., & Frier, H.I. (2003). Weight management using a meal replacement strategy: Meta and pooling analysis from six studies. International Journal of Obesity 27:537-549.
Phalan, S., Wyatt, H.R., Hill, J.O., & Wing, R.R. (2006). Are the eating and exercise habits of successful weight losers changing? Obesity 14, 710-716.
Pirozzo, S., Summerbell, C., Cameron, C., & Glasziou, P. (2003). Should we recommend low-fat diets for obesity? Obesity Review 4, 83-90.
Ross, R. (2009). The challenge of obesity treatment: avoiding weight regain. Canadian Medical Association Journal 180(10), 997-998.
Wing, R.R., & Hill, J.O. (2001). Successful weight loss maintenance. Annual Review of Nutrition 21, 323-341.
World Health Organization. (2000). Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation. Geneva, World Health Organization.