Introduction
When Young adults with mental health problems are nearing their adult years, they may face the difficulty of transitioning between juvenile and adult medical systems. Currently, there appears to be a mental illness in almost one in five young people that further might evolve into “homotypic and heterotypic disorders in adulthood” (Paul et al., 2018, p. 2). Overall, ethics in healthcare are vital as it leads to preserving, motivating, and maintaining patients’ dignity and moral integrity. The key issues arising in transitioning are over-reliance, paternalism, lost confidence, uncertainty about the quality of adult care, inadequate preparation for the transition, lack of privacy, and more (Paul et al., 2018). Thus, identifying the problem, defining the significance of the research question will represent the alignment of the topic with the Master’s Essentials.
The Problem and Its Significance
The transition between child and adolescent mental health services (CAMHS) to adult mental health services (AMHS) is a fundamental process essential to the healthcare system. The transitioning period takes place between sixteen and eighteen years old (Paul et al., 2018). Despite the developing number of studies intended to help the overall field of transitional nursing, little is thought about practices that bring about positive results or how moral issues are tended to (Bogossian et al., 2018). Not considering the transition from CAMHS to AMHS can lead to the deterioration of the patient’s diagnosis and the formation of a new one. The study by Paul et al., which was aimed at researching the literature on the ethics regarding the transition of young adults, indicated a lack of documentation on the topic (Paul et al., 2018). Therefore, the appropriate and ethical move to AMHS might give the advantage of fitting the emotional well-being of a mind and limit potential damage from untreated condition.
The present disjunction among CAMHS and AMHS makes foundational shortcomings in transitional nursing exactly when dangerous, dysfunctional behaviors start to develop, unjustifiably subverting progression of care exactly when it is required most. Moreover, the research demonstrates that CAMHS to AMHS transitional care is not uniform, as there seems to be a gap between the approach and practice (Paul et al., 2018). Therefore, broader research of the topic might be significant for improving nursing quality, which will eventually be beneficial for the patients’ recovery process. Moreover, improved-quality of research will lead to potential fundamental discoveries in transitional nursing, including among young patients with mental health problems, their caregivers, clinicians, program supervisors, and analysts. Overall, improving the nursing quality of young adults is extremely important, as it will help nurses be more professional, compassionate, and attentive to patients.
Purpose of The Research and Research Question
This is a mix study, qualitative and quantitative research. This study is necessary to preserve an informed ethical position in the face of an ever-increasing amount of scientific data of care and health services. Moreover, the research will help to endorse a high-quality transition and to accomplish a transfer of treatment from childhood into adulthood. There is not enough evidence to claim that ongoing nursing practices are effective (Paul et al., 2018). Thus, these imperfections increase the occurrence of damage and sabotage the reasonable arrangement of administrative work in nursing practices. On the other hand, young-adults sometimes decide not to enter the AMHS; therefore, the transition should be proposed ethically, not to underestimate the autonomy of a patient (Paul et al., 2018). Thus, the successful transition is not yet wholly defined from an ethical standpoint that would be both safe and convincing enough. Therefore, a research question is to study the moral aspect of CAMHS to AMHS transitional nursing in mental health patients. The research may be conducted by analyzing the existing nursing practices and strategies on the topic within various healthcare systems.
Master’s Essentials That Aligned with Your Topic
Master’s program empowers nurses in challenging, changing health systems, as well as training, and organizational structures for adaptable reasoning and strategic action. Master’s training provides nurses with useful experience and abilities to improve society, improve lives, and uplift treatment in multiple positions and areas. This research will align with Essential III, which is focused on improvement and safety (Barton, 2016). As this Essential stands for acknowledging that the nurse that is ready for the Master’s must be skilled in the quality-related processes, techniques, quality measures, and guidelines, and training to implement high-quality principles within an institution. Thus, learning more about the topic of ethics in CAMHS to AMHS nursing will incorporate learning more about techniques, tools, and ethical guidelines related to the problem. This research is connected to the sensitive topic of mental health, which will encourage the development of the necessary training and education.
Sampling and Reliability
Transitioning between child and adolescent mental health services (CAMHS) and adult mental health services (AMHS) is a complicated process. Multiple issues can arise during this process, which can lead to deterioration of the patient’s diagnosis. This mixed study is aimed at gaining a better understanding of these issues, their causes and potential changes to the transition that can help resolve them. Its results can be used to propose better moral and ethical standards for the transition.
Literature Review
The current research on the transition process from CAMHS to AMHS primarily focuses on issues related to specific diagnoses or health care contexts. A study by Lepièce, et al. (2019) provides background by showing that this age group is vulnerable to anxiety disorders. Cvejic & Trollor (2018), as well as Reale, et al. (2018) focus on ADHD and intellectual disability; both of these studies indicate issues with continuity of care between CAMHS and AMHS. These issues arise from limitations in the eligibility and poor transition planning (Cvejic & Trollor, 2018; Reale et al., 2018). Schraeder, et al (2019) points at the same gap in transition services. The systematic review by Paul, et al. (2015) further highlights the need for evidence on the subject and identifies more issues related to this transition gap. Most importantly, this review finds no clear evidence in favor of any particular model (Paul, et al., 2015). Finally, King, et al. (2020) describes the issues young people, especially those with autism spectrum disorders, face during the transition period. Although these studies do not propose any solutions, they identify a number of issues that occur during the transition period, as well as shortcomings in the associated medical pathways.
Methodology and Design
As this qualitative and quantitative study focuses on the moral and ethical issues that arise during the transition process between CAMHS and AMHS, it should gather a number of critical sets of data. First, transitional pathways need to be examined and collated to identify areas where such issues arise. To this end, practice guidelines and mental health policies need to be examined. Second, a survey aimed at practitioners must be created and administered to clinicians to identify the prevalent view on the relevant moral and ethical issues. Third, the transitioning patients’ perspectives and challenges must be assessed using a questionnaire aimed at them and their parents/carers, identifying their concerns and satisfaction. Finally, the results need to be compared against medical records to identify any correlations between one’s experience and treatment during the transition period to his or her outcomes. Furthermore, a follow-up study is advisable to evaluate changes in these outcomes after five or ten years.
The first survey’s questionnaire should focus on the decision making process of practitioners as they handle their patients’ transition. Thus, questions should concern the themes of difficulty in referring patients, challenges concerning informed consent and interactions with the patients’ parents/caretakers. The questionnaire for the second survey, aimed at the patients and carers, should discuss their experiences and their views on any issues that can arise during the transition period. Besides obvious questions related to satisfaction, factors such as patient/carer agency and self-efficacy need to be estimated. Specifically, the questionnaire should seek to determine whether the patients and carers felt that they had sufficient options for further treatment and were sufficiently informed about these options. This survey can be presented together with a patient satisfaction survey since it includes similar questions.
Sampling Methodology
As this is a non-intervention study focusing on a relatively small subset of the population, the most appropriate sampling method is a simple random sampling. Eligible subjects for the practitioner survey are chosen from those working in CAMHS and AMHS and have taken part in their patients’ transition process within the last 6 months. Patient and parent/carer subjects are chosen 6 to 12 months after their transition.
Necessary tools
The study centers on three separate surveys, are administered together. Each of these surveys should focus on one patient transition. The surveys should use a mixed format, primarily consisting of yes or no questions, but added numerical ranking and open-ended items. Listed are the critical items for each one of these questionnaires.
Survey 1: Practitioners
- When referring the patient to AMHC, were there any issues in providing the information necessary for the patient and his or her parents/carers o make an informed decision. (Yes/No)
- When referring the patient, were there any issues when determining to whom he or she should be referred? (Yes/No)
- How do you estimate the effect the transition process on the patient’s treatment progress (1 — significant deterioration, 10 — significant improvement).
Survey 2: Patients
- Were you unable to access any mental care facilities at any time during the transition period? (Yes/No)
- Did you experience anxiety from the transition process (1 — none, 10 — required medical intervention)
- Did you experience depression from the transition process (1 — none, 10 — required medical intervention)
- Did you have any difficulty understanding the details involved in the transition process (Yes/No)
- How satisfied are you with the care you receive at AMHC, compared to CAMHC (1 — much worse, 10 — much better)
Survey 3: Parents/carers
- Did you feel the information provided to you about the transition process was sufficient to make an informed decision? (Yes/No)
- How do you feel [the patient’s] diagnosis changed as a result of the transition (1 — significantly deteriorated, 10 — significantly improved)
Implementation Phase
During the first two phases, it was possible to identify the problem and locate its theoretical underpinnings. Apart from that, the previous two write-ups discussed the proposed methodology of the project as well as provided possible survey questions. The next phase of the project is implementation, whose efficiency is contingent on the engagement of all stakeholders and careful planning (LoBiondo-Wood & Haber, 2017). This paper discusses the implementation of the project starting from recruiting participants and ending with analyzing results and moving on to the next research goals. Besides, the current paper provides a comprehensive timeline of the project.
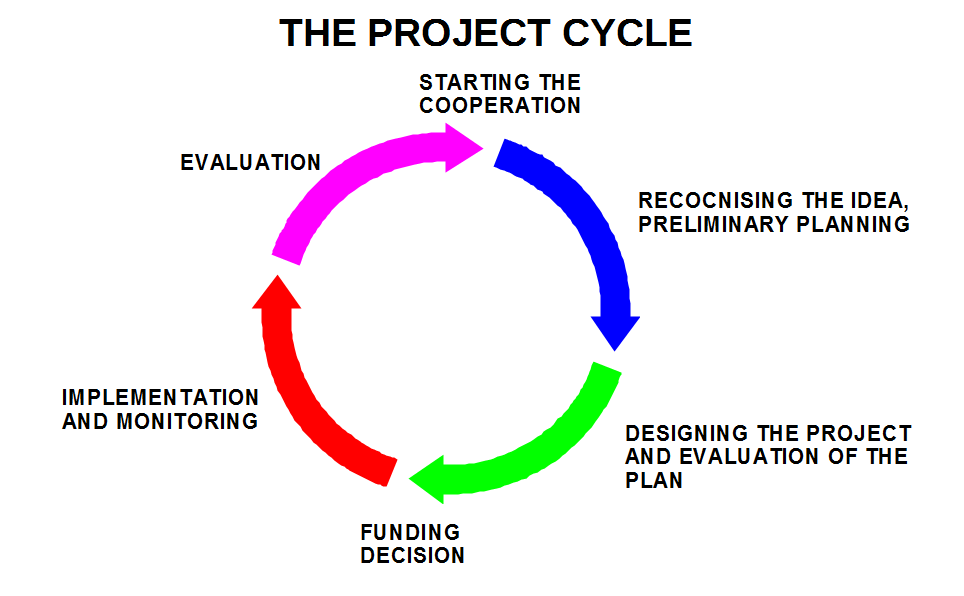
As seen from Image 1, the project is already past the “Recognizing the idea” and “Designing the project and evaluation of the plan” stages. The next stage is funding decisions: for any research project, it is critical to understand the associated costs. The current study is a non-invasion study that does not require any expensive equipment. The only resource that is needed is time resource; however, participants will not be offered a financial reward in order not to impact their motivation to share their experiences out of genuine interests. Hence, it is safe to conclude that the project’s costs will be negligible to none at all.
The next step is the implementation and monitoring, which in the case of the current project, encompasses recruitment and the administration of surveys. While the chosen sampling method for this project is random sampling, some eligibility criteria will be applied first such as working or partaking in CAMHS or AMHS within the last six months. It is expected that not every randomly selected person will consent to participation, which is why it makes sense to contact more people than necessary. Eventually, researchers will recruit twenty to fifty willing participants.
When doing human subject research, it is imperative to consider the ethical foundations of nursing research. Every human-subject study needs to comply with the four key healthcare ethics principles: autonomy, beneficence, non-maleficence, and justice (Doody & Noonan, 2016). For the current study, participants’ autonomy will be promoted through dissipation of information about research: its purpose, potential risks, and benefits (Doody & Noonan, 2016). The beneficence will be upheld through researchers’ commitment to the betterment of mental health services through making a contribution in the form of research. Non-maleficence will mean that none of participants will be hurt during the study’s administration or by its results: for instance, no-one will be criticized or punished for speaking out with honesty and frankness. Lastly, the principle of justice will ensure that all participants will be treated equally and no-one will be exposed to more risk than others.
Depending on how much time is given for the administration of the survey, it might make sense to administer a pilot survey first. Surveys may appear to be a simple quantitative research method when in reality, there are many pitfalls that can skew the end data (Lo-Biondo-Wood & Haber, 2017). The pilot study participants will be encouraged to provide feedback on whether some questions were too fuzzy or loaded or used unclear medical jargon. Some questions are planned to be open-ended for the collection of unstructured text data. Lo-Biondo-Wood and Haber (2017) point out that for surveys, it is not recommended to require participants to write a lot. If the pilot group speaks out about the inconvenience of writing, this part of the survey might be turned into an interview. The surveys themselves will be administered in study centers. While the online format has its own benefits, organizing a live session will allow for answering participants’ questions and, therefore, preventing ambiguity and misunderstanding.
The next stage will be data analysis, employing both quantitative and qualitative methods. For those questions that require choosing a number on a scale or answering Yes/ No, researchers will apply descriptive statistics such as mean, median, standard deviation, and others (Grove & Cipher, 2016). Within participant groups (patients, healthcare workers, and parents), it will also be possible to conduct factor analysis to understand differences in answers depending on participants’ characteristics such as age, gender, race, and others. As for qualitative data, it will make sense to conduct content analysis. This method will allow researchers to identify the key themes in unstructured data and find connections between them (Salvador, 2016). At the evaluation stage, the study results will be compared and contrasted to the existing body of research. Researchers will outline practical implications of the study and look into the ways of implementing them into the established workflow.
The timeline for the current project will look as follows:
- Week 1-2: participant recruitment;
- Week 3: pilot study;
- Week 4: pilot study results and feedback evaluation, adjustment to survey questions;
- Week 5-6: administration of surveys in study centers;
- Week 6-7: statistical analysis of the data, its visualization, and evaluation;
- Week 8: presentation of results, dissipation of new knowledge;
- Week 9: considering the study’s practical implications.
- Five-ten years after the initial study: a follow-up survey.
Results
This mixed paper discusses the results of the hypothetical analysis and the statistical tools used in the research and its limitations. The outcomes of the study are inferred from the formalized interview conducted with three groups of respondents: practitioners, patients, and people who take care of the previously mentioned group of interviewees. The results of the current research indicate that the quality of transitioning nursing is rather poor and requires improvements.
Descriptive Data
The population was chosen randomly from the appropriate sample that satisfies the criteria mentioned in the preceding phase of the research paper. Out of 30 respondents, 35 percent were women and 65 percent were men. The age of the polled varied from 18 to 65. The average of patients was 20.5 years. The respondents are US citizens but came from various parts of the country.
Results of the Survey
At this point, one could argue that a small population size harms the research and makes its results untrustworthy. Nevertheless, this opinion is debatable since it is up to the investigator to decide which size of the sample to choose (Boddy, 2016). Each group out of three being surveyed consists of 10 interviewees.
Concerning the examination of practitioners, it should be mentioned that eight out of ten admitted that they could not provide the patient with all the necessary information on Adult Mental Health Services (AMHS). Besides, the overwhelming majority of the respondents answered that they did not know to whom referred the patient in case of any issues. Mulvale et al. (2016) suggest that the reason for this situation lies in the fact that the staff members of the Child and Adolescent Mental Health Services (CAMHS) are not familiar with the specificity of work in AMHS. Finally, half of the practitioners replied that the transition from CAMHS to AMHS did not affect the progress of the patient. At the same time, another half of the respondents told that the patient had a slight deterioration in the treatment progress.
The results of the survey conducted among 10 patients also confirm that the present system of shift from CAMHS to AMHS requires improvements. Although only three out of ten patients after transition became unable to access the required mental care facilities, nine interviewees acknowledged that they experienced anxiety and depression because of the transition. Gulpers et al. (2016) note that the sense of fear stimulates cognitive decline. Therefore, from this it follows that the previously mentioned observation on the decline of the patients treatment progress is partly based on the stress and anxiety they feel during the transition process. These aspects, as well as the difficulties with understanding of details of the move, resulted in dissatisfaction with the care in AMHS admitted by 60 percent of the polled.
The survey of the thirds group (patients parents or caretakers) also confirmed the previously mentioned apprehensions on the quality of transition nursing in young adults. 80 percent of respondents possessed limited information concerning the discussed topic. 4 out of 10 polled told that they regard the period of transition as a driving force for the decline in the treatment success of the patient.
Research Limitations
Due to the population size, results can be interpreted as bias. Another limitation is the decision to examine only the medical staff who works in CAMHS. The inclusion of specialists from AMHS would help to examine the issue of transition from a different perspective and make the study more comprehensive. Finally, the current research is based on non-inclusion in the affairs of the services. Therefore, it is advised to select an experimental group in which the practitioners from CAMHS and AMHS would cooperate and ask the same questions the same groups of respondents. This option would make the research multidimensional and would help to indicate whether relations between the representatives of the two services is the key to more successful patients transition process.
Learning Experiences
This research produced valuable learning experiences that align closely with the essentials of a Master’s education in nursing. In particular, as mentioned above, the issue at the center of the research coincides with Essential III: Quality Improvement and Safety. American Association of Colleges of Nursing (2011) states that a nurse with a master’s degree “must be articulate in the methods, tools, performance measures, culture of safety principles, and standards related to quality” (p. 13). The results of the research highlight that 8 out of 10 practitioners examined admitted being unable to provide full information on Adult Mental Health Services (AMHS). Moreover, as mentioned above, not every practitioner was sure whom to refer the patient to for further clarification. These results demonstrate that not every nurse in the field of child and adolescent mental health services (CAMHS) is articulate enough in the methods, tools, and principles employed in Adult Mental Health Services (AMHS). Thus, conducting the research provided a learning experience that emphasizes the importance of quality improvement and safety as an essential of a Master’s education in nursing and pinpoints a specific area where it can be improved.
Apart from the essentials of Master’s education in nursing, the research also provided learning experiences that pertain closely to the course. Although the study was not implemented in practice, writing the paper contributed to several associated skills. To begin with, it provided an experience of designing research and, in particular, combining qualitative and quantitative methods thus giving a better insight into the planning phase (“NGR 5110,” 2020). It also offered an experience of elaborating on the implementation of research, including the development of a week-by-week timeline and designated follow-up. Additionally, the development of the hypothetical step-by-step implementation process highlighted the awareness about the ethical foundations of human subject research and other important concerns that pertain to conducting nursing research (“NGR 5110,” 2020). Finally, even though the study was not implemented in practice and the results were purely hypothetical, it still offered an experience of recognizing and pointing out research limitations of a given study. Therefore, this research project provided a number of learning experiences that relate closely to the course syllabus and contribute to a better understanding of designing, conducting, and reporting on nursing research.
Conclusion
Young adults with mental health problems may encounter considerable difficulties when transitioning from child and adolescent mental health services (CAMHS) to Adult Mental Health Services (AMHS), potentially resulting in the deterioration of the patient’s diagnosis. Nursing is essential for a high-quality transition, but the current evidence of the efficiency of the process is insufficient. This mixed study involving practitioners, patients, and parents/caregivers confirms the existence of continuity issues with the patients transitioning from CAMHS to AMHS. These include the practitioners’ inability to inform the patients about AMHS in the majority of cases and the slight deterioration in the patient’s condition in half of the cases. The results highlight an issue with the transition from CAMHS to AHMS and suggest that the inefficient transition may be the driving force behind the deterioration in young adults facing mental health problems. The sample size and the fact that the research is limited to the practitioners from CAHMS are the major limitations of the present study. Further research with participants from both AHMS and CAHMS and, potentially, a greater sample, is advisable.
References
American Association of Colleges of Nursing (2011). The Essentials of Master’s Education in Nursing.
Barton, A. J. (2016). Teaching Health Centers: A Possible Model for Nursing Education. Journal of Nursing Education, 55(10), 547–549.
Bogossian, A., Gorter, J. W., & Racine, E. (2018). Protocol for a scoping review about ethics in transition programmes for adolescents and young adults with neurodisabilities. BMJ Open, 8(8).
Boddy, C. R. (2016). Sample size for qualitative research. Qualitative Market Research: An International Journal, 19 (4), 426-432.
Cvejic, R. C., & Trollor, J. N. (2018). Transition to adult mental health services for young people with an intellectual disability. Journal of Paediatrics and Child Health, 54(10), 1127–1130.
Doody, O., & Noonan, M. (2016). Nursing research ethics, guidance and application in practice. British Journal of Nursing, 25(14), 803-807.
Embrett, M. G., Randall, G. E., Longo, C. J., Nguyen, T., & Mulvale, G. (2015). Effectiveness of health system services and programs for youth to adult transitions in mental health care: a systematic review of academic literature. J Ment Health Pol Econom, 18, S12-S3.
Gulpers, B., Ramakers, I., Hamel, R., Köhler, S., Voshaar, R. O., & Verhey, F. (2016). Anxiety as a predictor for cognitive decline and dementia: a systematic review and meta-analysis. The American Journal of Geriatric Psychiatry, 24(10), 823-842.
Grove, S. K., & Cipher, D. J. (2016). Statistics for Nursing Research-EBook: A Workbook for Evidence-Based Practice. Elsevier Health Sciences.
King, C., Merrick, H., & Le Couteur, A. (2020). How should we support young people with ASD and mental health problems as they navigate the transition to adult life including access to adult healthcare services. Epidemiology and psychiatric sciences, 29, e90.
Lepièce, B., Zdanowicz, N., de Becker, E., de Timary, P., & Lorant, V. (2019). Adolescents in transition to young adulthood: evolution of mental health status and risk factors associated with depressive and anxiety disorder. Psychiatria Danubina, 31(Suppl 3), 371–375.
LoBiondo-Wood, G., & Haber, J. (2017). Nursing research-ebook: Methods and critical appraisal for evidence-based practice. Elsevier Health Sciences.
Mulvale, G. M., Nguyen, T. D., Miatello, A. M., Embrett, M. G., Wakefield, P. A., & Randall, G. E. (2016). Lost in transition or translation? Care philosophies and transitions between child and youth and adult mental health services: a systematic review. Journal of Mental Health, 28(4),1-10.
NGR 5110 Course Syllabus. (2020). Adobe PDF File.
Paul, M., Street, C., Wheeler, N., & Singh, S. P. (2015). Transition to adult services for young people with mental health needs: A systematic review. Clinical child psychology and psychiatry, 20(3), 436–457.
Reale, L., Costantino, M. A., Sequi, M., & Bonati, M. (2018). Transition to Adult Mental Health Services for Young People With ADHD. Journal of attention disorders, 22(6), 601–608.
Schraeder, K. E., Reid, G. J., & Brown, J. B. (2019). An exploratory study of children’s mental health providers’ perspectives on the transition to adult care for young adolescents in the Canadian context. Journal of Pediatric Nursing, 49, 51–59.
Salvador, J. T. (2016). Exploring quantitative and qualitative methodologies: A guide to novice nursing researchers. European Scientific Journal, 12(18), 107-122.
Shirley, D. (2020). Project management for healthcare. CRC Press.
Paul, M., O’Hara, L., Tah, P., Street, C., Maras, A., Ouakil, D. P., Santosh, P., Signorini, G., Singh, S. P., Tuomainen, H., McNicholas, F., & Milestone Consortium. (2018). A systematic review of the literature on ethical aspects of transitional care between child- and adult-orientated health services. BMC Medical Ethics, 19(1).