Problem Statement
Current medicine is slowly but steadily becoming focused on working efficiency, minimizing patient stay at the clinics, and teaching personnel to handle multitasking. It is believed that a healthcare professional that can provide various services to the patients is most effective and needed at the working place. However, in real life, the actual flow of events differs from this ideal picture. Healthcare providers experience burnouts, low attention, and extra hours of work because of the economizing and rational approaches. The number of staff is shortened; however, it is hard to predict the complicity of the condition of every patient, especially in acute care units. Some nurses spend most of their working time on one or two patients barely managing their care and controlling the medications, monitors, and treatment outcomes. It is mostly a nurse’s responsibility of providing high-quality care and report acute situations to the physicians. In 2019, it was estimated that six million people worked as a nurse in the U.S., and that was the largest segment of the healthcare workforce (Shah et al., 2021). That is why nurse staffing questions have to be considered thoroughly by each healthcare unit to provide them with decent working norms, legislation, and rest.
Safe nurse staffing is a significant issue for patient safety and the quality of care in hospitals, communities, and all settings in which care is provided. International Council of Nurses (2018) reported that inadequate or insufficient nurse staffing levels increase the risk of compromised care and adverse events for patients. Issues with nurse staffing also lead to inferior clinical outcomes, in-patient death, and poorer patient expertise of care. Having fatigued nursing staff to meet patient needs also results in unsustainable workloads and negatively impacts the health and well-being of staff.
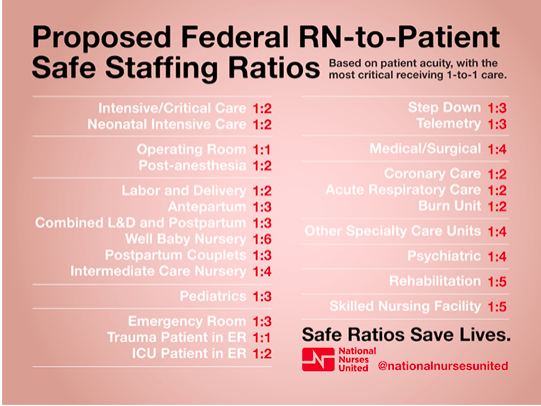
According to several studies, the expense of recruiting more nurses will put a strain on hospitals’ finances if state legislators mandate minimum nurse staffing ratios. According to other studies, investing in safe, effective, and needs-based nurse staffing levels can be cost-effective and prevent deterioration in patients’ health, thereby reducing the duration and intensity of healthcare interventions (Juvé-Udina et al., 2020). To solve this problem, federal nurse-to-patient ratios were developed assessing patient acuity and healthcare units the healthcare is provided. According to the Federal ratios, in intensive or critical care, one nurse can monitor two patients’ conditions, and rehabilitation units, for instance, need one nurse to address five patients (National Nurses United, 2021). Not all the states accepted the Federal ratios which make the work experience of nurses throughout the country diversified. The full list of sage nurse staffing ratios is presented below.
The burnout of nursing professionals is another major reason for having poor service and treatment outcomes. In workplace settings, hours of work per week directly impact the will or decision of nursing personnel to quit the job (Shah et al., 2021). Generally, healthcare professionals are one of the highest risk groups to experience burnouts, and several norms and rules should regulate this fact. Nurses control various tasks including health promotion, treatment monitoring, effective communication with physicians, organizational leadership within working environments, disease prevention, and many others. After COVID-19 pandemics, nurses were required to have more skills and manage multitasking because of patients’ numbers and a variety of their conditions and needs. All these factors unite in working environment complication and faster burnouts of the personnel. Burnouts among health working professionals lead to ineffective treatment outcomes and increased risk of mistakes. Mandatory policies securing adequate nurse-to-patient ratios depending on the department, can improve the patient’s length of stay in one year, their treatment outcomes, and normalize the working regime of nurses.
The current research will implement such policies to the staff of Atrium Health Hospital and assess the outcomes of normalized RN-to-patient ratios on in-patient length of stay. The hypothesis of the research is the enhancement of treatment outcomes and shortening of clinic’s expenses after the extra recruitment and better planning of nursing working hours at the Atrium Health Hospital. The research aims to prove the efficiency of the hospital statistics after providing a safer and more adequate working environment.
Organizational Culture and Readiness
Organizational culture is about the shared ways in which employees in an organization think, feel, and behave. Organizational culture and readiness are about measuring the readiness of a healthcare organization to go through a major change or take up a new project (Miake-Lye et al., 2020). Atrium Health Hospital has an organizational culture that supports change, and it has a very clear business strategy of “safe, compassionate, and quality healthcare services” (Atrium Health, 2022). This strategy is supported by almost everyone working in the organization. Employees at the Atrium Health Hospital know their roles and responsibilities and how it affects their organization. The leadership team at Atrium Health Hospital is always at the forefront when it comes to implementing change in the organization, establishing accountability at all levels of the organization, in defining the results from culture change. The leaders of the hospital are good at developing and communicating the need for change. The management at the clinic has devised effective communication, learning, and reinforcement systems that would continually stress behaviors and practices that are necessary to speed up change and implementation.
The organization readiness tool selected to assess the readiness for change is the Organizational Readiness to Change Assessment (ORCA) which helps to investigate, evaluate, and identify the readiness of the organization to implement the evidence-based practice. The latter represents the approach to the treatment and care that relies on unified data of up-to-date research, clinical expertise, and patient benefit.
There is a need for commitment, knowledge, and ongoing learning among healthcare professionals so that evidence-based practice is always useful in healthcare units. The organizational culture at Atrium Health Hospital would sustain a change in evidence-based practice by motivating healthcare professionals to enhance the level of their education. With the help of innovative programs and tools based on EBP, healthcare staff can upgrade their skills, simplify the working environment, and prevent burnouts that eventually can lead to improved patient outcomes. Atrium Health Hospital would also strive to educate the staff on the ways of effective communication between each other and specialties of psychological conditions that might signalize chronic stress and tiredness. The strengths that can impact the implementation of the EBP at Atrium Health Hospital are good organizational leadership and increased access to information.
However, the weakness is the lack of time nurses face due to the higher workload. Understanding and learning a new approach and system that can be implemented in the working environment requires an extra amount of time, rest, and preparedness. This means the hospital leaders should plan and schedule the studying hours involved in the working shift of the personnel. The other barriers to the successful EBP implementation are poor knowledge regarding the use of the EBP by healthcare service providers, and inexperience of the EBP usage by the healthcare staff. The personnel of various ages has different skills and attitudes to the innovations and electronic assessment tools. Checking the outcomes of EBP teaching and increasing readiness of the staff to learn can correlate with the general level of new data understanding. Therefore, to ensure readiness for change at Atrium Health Hospital, the stakeholders and the leaders of Atrium Health Hospital should get engaged to ensure the implementation of the new project proposal. Stakeholders such as nurse educators, nurse managers, and physicians should work with nursing staff and realize the implementation of the EBP in the clinical environment.
The duties of the nurse manager are to justify changes in evidence-based practices by discussing the practices with staff nurses, share information with them through written instructions, and facilitate education and training of staff nurses about the EBP project (Caramanica & Spiva, 2018). The duties of a physician in EBP are clinical thinking and information synthesis, searching for relevant medical literature, and uploading the patient history in the database so that other people can get access to it if needed. The duties of nurses are to implement innovative tools and teach the other personnel about innovative services and communication tools.
According to EBP, the hospital will be taught and recommended to implement systems detecting cases of overtreatment as it leads to avoidance of wasteful expenditure and provision of safe and quality care to patients. Clinical errors done by overworked or burnout doctors and nurses can be escaped by having up-to-date tools and systems tracking the doctoral mistakes and proposing possible solutions to the issues. Cutting down on such clinical errors through the administration of best practices and services can help the clinic save costs on prolongation of patient’s treatment, extra medication prescription, and extra working time of personnel.
Information and Communication Technologies (ICTs) such as Electronic Health Records (EHR) and computerized nursing plans help the staff access patient information easily and plan working processes. Electronic Health Records (EHR) is a systemized base that allows to improve the communication and information sharing between the staff without breaking patient’s rights and simplify administrative processes between providers and payers (Acharya & Werts, 2019). Nurses should shift to electronic health systems that record patient information in a database. Stakeholders can integrate ICT in planning a roadmap through budget planning, scheduling, data transfer, training of hospital staff. The successful implementation of information communication technologies includes performing many tests on the ICTs before implementing them and checking if the ICT meets all the requirements of the healthcare organization (Acharya, 2019). Moreover, the leaders should move legacy data to the new database, provide training to relevant healthcare staff, and troubleshoot the system for any errors that may occur at the time of integrating the system (Acharya, 2019).
ICTs such as an EHR can help improve nursing practice and care delivery through reduction of documentation errors, improving patient safety, and reaching better patient outcomes. EHR keeps a record of patient medication and allergies and checks if there are any intersections when a new medicine is prescribed (Blumenthal et al., 2017). Following this plan, ICTs such as EHR help improve nursing practice and care delivery for individuals and populations.
Literature Review
Hospital nursing staff delivers holistic treatment and care to the patients, and it is essential to care about their working norms. The study by Shin, Park, and Bae (2018) estimated the correlation between a greater nurse-to-patient ratio and their burnouts, job dissatisfaction, and patient outcomes. The use of nurse overtime, recruiting temporary nurses can aggravate the shortages of nursing personnel and worsen their perception of the working environment. The researchers state that regulation of nursing staffing should be central in healthcare providers as this segment of professionals is most skillful and needed at the hospitals (Shin, Park & Bae, 2018). In the United States of America, several states have already implemented nursing staff policies. For instance, California incorporated nurse-to-patient ratios, Texas implemented mandated nurse staffing committees, and New York mandated disclosure of hospital nurse staffing levels (Shin, Park & Bae, 2018). Based on the findings, the increase in RN-to-patient ratio was directly correlated with nurse job dissatisfaction, risk of burnouts, and worsened patient treatment results (Shin, Park & Bae, 2018). Thus, providing protection and normalization of the nurse occupation with patients can significantly improve the quality of healthcare.
The latter can seriously lead to the increased stress of nurses at the working place due to time scarcity and missed nursing activities. Employees with high responsibility levels tend to develop high levels of stress and consequent unproductiveness at work due to inadequate staffing. It was proved that missed nursing care substantially worsened patient safety, unfavorable events, increased mortality ratio and lowered levels of patient satisfaction (Cho et al., 2019). The authors of the study implemented in South Korean hospitals suggested that inadequate care can relate to the scope of nurses’ responsibility (Cho et al., 2019). According to the results of the research, the nurses responsible for basic care reported better care outcomes than those who were involved in multitasking, medication, and documentation processes (Cho et al., 2019). Another work proved the deterioration of nursing healthcare because of the low RN staffing. Smith et al. (2020) emphasized the incapability of nurses of the acute care hospital in England to respond to the abnormalities in patients’ vital signs (Smith et al., 2020). The ability to perform in acute settings is a fundamental aspect of nursing and an essential contributor to patient safety. This means adequate staffing might help escape from missed nursing activities and separating nursing responsibilities can enhance their performance outcomes. Recruiting more staff can reduce the stress levels of nurses and their perceptions of multitasking and responsibilities at work.
Increased mortality rates were also proved by a Swiss study assessing the work of nursing personnel and their staffing. Musy et al. (2021) proved that patients benefit from high registered nurse staff shifts. On the contrary, low registered nurse shifts correlated with such patient complications as nosocomial infections, falls from beds, and mortality (Musy et al., 2021). This study proves the importance of nurse staffing regulation and identifies the major risks for the patient and the healthcare unit.
Another study was conducted by Butler et al. (2019) about hospital nurse-staffing models and patient and staff-related results. The study was to explore the effect of hospital nurse staffing models on patient and staff-related outcomes in the hospital setting, specifically identifying which staffing models are associated with better results for patient care, better staff-related outcomes, and the impact of the staffing model on cost outcomes. Butler et al. (2019) reported that the study suggested interventions related to hospital nurse staffing models to improve patient outcomes, clearly adding specialist nursing and specialist support roles into the nursing workforce. On the other hand, Shin et al. (2018) reported that a higher nurse-to-patient ratio is related to adverse nurse outcomes.
Change Model, or Framework
Applying a model ensures that a process is in place to guide the efforts for change with the help of the Iowa model framework. The latter helps guide nurses to utilize research findings to improve patient care. The Iowa model shines a light on knowledge, problem-focused triggers, collaboration, and organization using research. The model is relevant since it promotes quality care based on EBP. The steps of the Iowa model involve identifying the topic and triggering issues, stating the purpose, building a team, assembling, appraising, and synthesizing a body of evidence, designing and piloting the practice change, integrating and sustaining the practice change, and disseminating the results.
The topic of the current research is poor nurse staffing as a reason for worsened patient care and their prolonged stay at the hospital. Triggering issues are temporal nurse recruitment, working overtime, multitasking, time pressure, hospital policies, and burnouts. To fight these triggers, hospitals should implement EBP and improve organizational structure and working environment. The purpose is to spread and implement federal norms of nurse-to-patient ratios throughout the U.S. so that the working norms of nurses will be equal. Another purpose of the study is to implement at the hospitals at the example of Atrium Health Hospital evidence-based practice and improve communication skills between staff, working schedule, and shift regulation. A team of educators, nurse managers, and physicians should work with nursing staff and realize the implementation of the EBP in the clinical environment. The leader of the clinics should understand that every change requires energy, time, and effort. Developing readiness and better working schedules for personnel to learn and insert innovative tools might help this process.
The evidence will be gathered from patient-to-nurse ratios and personnel and patient interviews. The synthesis of the data can allow estimating the outcomes of better nurse staffing and the feedback from the employees and healthcare receivers. Within one year of normalization of nurse staffing at Atrium Health Hospital, the patient duration of stay, their treatment outcomes, and general care satisfaction will be estimated to analyze the impact of the staffing factor on general nursing care. The hospital can only sign long-term contracts and try to avoid temporary nurse recruitment during the research period. There should also be guidance for piloting the practice change and developing an implementation plan and preparing clinicians and materials to reach the needed planned change.
The team identifies and engages vital personnel as integration needs new change leaders and groups. Incorporating this stage of integration creates linkages with the governance structure, promoting the right influence required from senior leadership. It means embedding a new practice into the organization. The results can be published internally, and lessons learned can be shared externally. The evidence should show that it can contribute to patient care. The team members should conduct audits and feedback. The members can assess the program’s impact and consistency against an actual change with the desired effect through evaluation.
Implementation Plan
The implementation plan is a complicated process that incorporates a variety of professionals, phases, difficulties, as well as drivers. The nursing profession and the healthcare system as a whole rely heavily on the correct number of caregivers to perform their duties. The ability of these individuals to offer safe and high-quality care in a variety of practice settings is influenced by the number of nurses available. For the sake of everyone’s health, the enrolment authorities must abandon damaging recruitment practices and policies (Shin et al., 2018). To improve wellbeing and health care delivery, one must ensure the safety of the employees and provide the best in evidence-based policy and preparation as well as professional development.
The proposed policies will be implemented in five different departments of a specific healthcare facility (Atrium Health Hospital). All ethical norms of research shall be carefully adhered to throughout the process. During the next two weeks, there will be extensive advertising to ensure that as many nurses and other healthcare professionals as possible are aware of the projected regulations to enhance the nurse-to-patient staffing ratio in healthcare facilities. The consent would be sought from all registered nurses as well as other stakeholders who will be arguing for the necessity for the implementation of policies that increase patient-nurse staffing ratios. These opinions will have to be included in the approval of the required policies. A week before the guidelines are implemented, the subjects engaged will have to be trained in their respective fields of expertise. In addition, the opinions of healthcare administrators will be solicited to ensure that the project is consistent with the mission, vision, and goals of the healthcare facility.
A particular time limit is required to implement mandatory regulations to address understaffing in medical care facilities. In this regard, it will take three months to enforce all the rules that have been suggested in the five departments involved. To ensure that all procedures are applied and assessed to determine the degree of outcomes, the time frame proposed is more than sufficient. The general time for data gathering is one year of clinical practice during which the patient outcomes and the patient and nursing feedback will be collected.
Throughout the execution stage, appropriate resources are required to guarantee a seamless application procedure. Resources are necessary to enable work during the implementation stage. This technique involves the establishment of a budget to cover the costs of essential resources. The enactment step is the costliest and has failed numerous change projects due to resource constraints. To implement the suggested policies, the following capitals will be required: a human capital to teach nurses on the application process, laptops and desktops for presentation, projectors, print-out papers, VGA cables, and projector screens. Additionally, conference rooms will be necessary to accommodate the number of persons attending the proposed policies’ awareness program. The budget for all essential resources is projected to be $35000. If the projected budgeted money is achieved, all the operations will run smoothly.
Throughout the one-year duration of the study’s data-collecting phase, a questionnaire will gather data constantly. Participants will provide information on their progress following the intervention and answer questions on the interview regarding their new staffing. Each week, participants will complete a form containing the outcome of an implemented policy that was incorporated within the department. The results will demonstrate the intervention’s efficiency in increasing the nurse-patient staffing ratio and enhancing patients’ results. Statistics will also be collected and recorded into excel spreadsheets. After the study is completed, the other step will be interpretation and analysis. The information gathering form will be similar to the one used for implementation monitoring.
The policies that have been advocated will be executed in an integrated manner. Several primary interventions will be implemented, including raising awareness of newly developed policies that should be adopted, disseminating printed copies of comprehensive policy documents, applying procedures in departments, and requesting feedback on the policies’ applicability. Participants will get instruction regarding the guidelines as to the way they will be implemented in inpatient care, and how to adhere to them before they are executed. Every week, a group of individuals will be selected to provide an update on the progress of implementation. Using this information, one may determine the effectiveness and credibility of the procedure. In principle, the project is concerned with putting into effect suggested guidelines that, if followed, will likely improve nurse-to-patient ratios and, as a result, reduce the length of time patients spend in acute care hospitals.
Evaluation Plan
The nurse-to-patient staffing ratio is a critical subject for delivering healthcare services to patients. The ratio determines the outcome of the clinical services, and it makes it easy to weigh the model in which healthcare services should be regulated (Griffiths et al., 2018). Some legislative models empower nurses to create staffing frameworks specific to each workstation. The expected outcome is that the research will have concrete findings that can be useful to combat nurse staffing issues. There is an expectation that increasing the nurse-to-patient ratio decreases the risk of adverse effects of patients admitted to hospitals. From the proposal, the content will be useful to have a rationale for why the number of nurses in a given hospital setting determines the outcome of the clinical delivery of healthcare services.
Various data collection tools can be useful for correlational research. The first option is using a questionnaire whereby respondents give answers to questions provided in the forms. Second is the use of the audio recorder to capture important concepts that are gotten from interviews. Collecting data by interviews gives the respondent primary information, which ensures there is no manipulation of data during presentation and analysis. The last data collection tool that fits this research design is the use of hospital care records. The reason is that health care has new ways of collecting data electronically. Therefore, a researcher can rely on the information systems used in hospitals to analyze and present the problem being researched. For example, these records can show the rate of nurse turnover and the occupancy of the clinic or hospital where the latter used to work (Griffiths et al., 2018). This must be obtained under legal measures to ensure the nursing ethics are not breached.
The most effective data collection tool, in this case, is the use of questionnaires to healthcare workers and also the patients who have experienced insufficient clinical care when hospitalized. The tool is important because it gives broad information and the extent to which the nurse-to-patient ratio is impactful on the clinical care of patients. The reliability of questionnaire forms is that the researcher can ask a uniform set of questions, and anything in contention can be checked during a pilot study. Questionnaire forms can be valid because the researcher may ask closed questions that limit the respondents’ answers. The accuracy of the data can be ascertained by comparing answers given with the reports on staffing of nurses. Thus, the nurse staffing issue would be easy to investigate based on the above metrics.
The appropriate statistical test to use for this study is the Pearson correlation coefficient. The test is suitable because it determines the relationship between nurse staffing ratios and the improvement of patients’ length of stay. The Pearson test shows the degree to which the variables coincide with each other (Xu & Deng, 2018). The changes in nurse staffing ratios correspond to the alteration of improved patient length of stay. Through the test, it is easy to ascertain the rate at which adding or reducing the nurses in a given hospital setting will affect the chances of patients improving from the conditions.
The outcome will be measured by the number of patients who show improvement under care that has enough nursing staff compared with the low nurse-to-patient setting (Griffiths et al., 2018). Through the responses given, it will be possible to know what effect reducing or adding nursing staff has to do with patient recovery in a short time. The answers to questions shall be the checklist when determining the outcome of the matter.
Thus, this research can show the strengths and weaknesses of a given clinical framework at the hospitals. This empowers healthcare professionals to enact in a desirable way to combat any adverse changes. It is also possible to evaluate performance through a broad-based approach that identifies a range of EBP impacts. In that way, it would be easy to make decisions that can prevent the escalation of problems relating to the nurse-to-patient ratio in relation to improved patient care.
References
Acharya, S., & Werts, N. (2019). Toward the design of an engagement tool for effective electronic health record adoption. Perspectives in Health Information Management, 16, 1g.
Atrium Health (n.d.). Strategy and transformation office. Web.
Blumenthal, K. G., Acker, W. W., Li, Y., Holtzman, N. S., & Zhou, L. (2017). Allergy entry and deletion in the electronic health record. Annals of Allergy, Asthma & Immunology, 118(3), 380. Web.
Butler, M., Schultz, T. J., Halligan, P., Sheridan, A., Kinsman, L., Rotter, T., Beaumier, J., Kelly, R. G., & Drennan, J. (2019). Hospital nurse‐staffing models and patient‐and staff‐related outcomes. Cochrane Database of Systematic Reviews, 4, CD007019. Web.
Caramanica, L., & Spiva, L. (2018). Exploring nurse manager support of evidence-based practice: Clinical nurse perceptions. JONA: The Journal of Nursing Administration, 48(5), 272-278. Web.
Cho, S.-H., Lee, J.-Y., You, S. J., Song, K. J., & Hong, K. J. (2020). Nurse staffing, nurse’s prioritization, missed care, quality of nursing care, and nurse outcomes. International Journal of Nursing Practice, 26(1), e12803. Web.
Griffiths, P., Recio-Saucedo, A., Dall’Ora, C., Briggs, J., Maruotti, A., Meredith, P., Smith, G. B., Ball, J., & Missed Care Study Group. (2018). The association between nurse staffing and omissions in nursing care: A systematic review. Journal of Advanced Nursing, 74(7), 1474–1487.
International Council of Nurses. (2018). Evidence-Based safe nursing staffing. Web.
Juvé-Udina, M.-E., González-Samartino, M., López-Jiménez, M. M., Planas-Canals, M., Rodríguez-Fernández, H., Batuecas Duelt, I. J., Tapia-Pérez, M., Pons Prats, M., Jiménez-Martínez, E., Barberà Llorca, M. À., Asensio-Flores, S., Berbis-Morelló, C., Zuriguel-Pérez, E., Delgado-Hito, P., Rey Luque, Ó., Zabalegui, A., Fabrellas, N., & Adamuz, J. (2020). Acuity, nurse staffing and workforce, missed care and patient outcomes: A cluster-unit-level descriptive comparison. Journal of Nursing Management, 28(8), 2216–2229. Web.
Miake-Lye, I. M., Delevan, D. M., Ganz, D. A., Mittman, B. S., & Finley, E. P. (2020). Unpacking organizational readiness for change: An updated systematic review and content analysis of assessments. BMC health services research, 20(1), 1-13.
National Nurses United (2021). National campaign for safe RN-to-Patient staffing ratios. Web.
Shah, M. K., Gandrakota, N., Cimiotti, J. P., Ghose, N., Moore, M., & Ali, M. K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA network open, 4(2), e2036469-e2036469. Web.
Shin, S., Park, J. H., & Bae, S. H. (2018). Nurse staffing and nurse outcomes: A systematic review and meta-analysis. Nursing Outlook, 66(3), 273–282. Web.
Smith, G. B., Redfern, O., Maruotti, A., Recio-Saucedo, A., Griffiths, P., & The Missed Care Study Group. (2020). The association between nurse staffing levels and a failure to respond to patients with deranged physiology: A retrospective observational study in the UK. Resuscitation, 149, 202–208. Web.