Abstract
Type 2 diabetes mellitus is a serious metabolic condition that is affecting large portions of the population and growing at an increased rate. The disease affects virtually all demographics but is associated with overweight and obesity as risk factors. Individuals with type 2 diabetes typically have issues with dietary patterns and appropriate nutrition which impacts glycemic control and results in cell inflammation and organ deterioration in the long-term with a wide range of health consequences such as heart disease, cancer, and neuropathy. Strategies to improve nutritional intake in order to prevent or manage type 2 diabetes focus on patient education and public health programs which emphasize dietary habits. Nutritional quality, particularly in diets with more wholegrains, legumes, and fruits/vegetables are effective in creating weight loss, and subsequently glycemic control for the management of diabetes mellitus. The issue of type 2 diabetes prevalence is just as much cultural as it is health-associated. There must be targeted programs and policy aimed at addressing the underlying problems such as high sugar content in modern foods, emphasis on prepackaged foods, and access to fresh foods among high risk populations. These and other measures discussed in this paper are aimed at potentially decreasing type 2 diabetes incidence and reduce the health and socio-economic burden of the disease on the population.
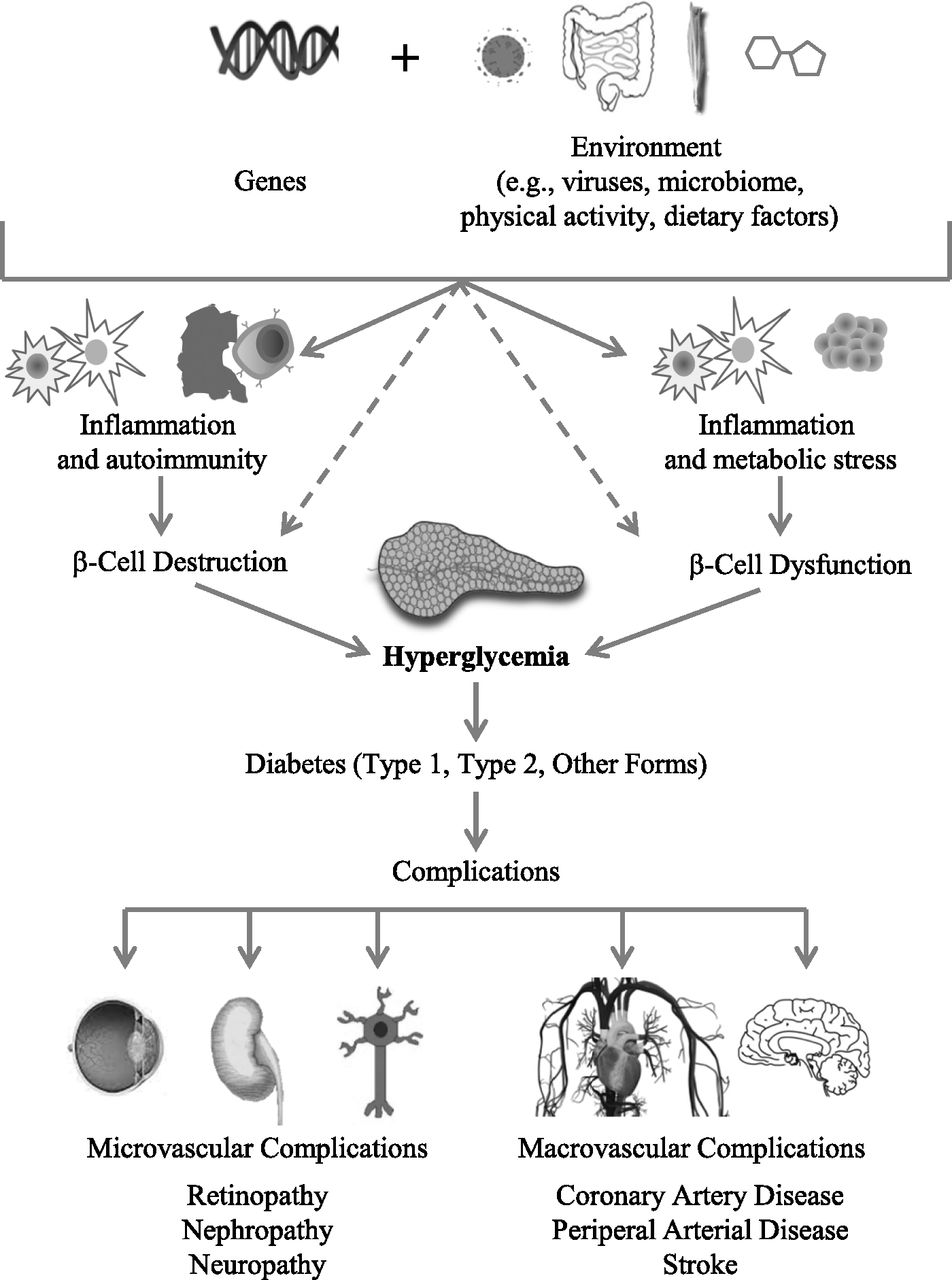
Type II diabetes mellitus (referred periodically in this paper as simply ‘diabetes’) is a non-infectious chronic disease that is becoming increasing prevalent around the world. Type II diabetes has severe health impacts with both short- and long-term consequences as well as being linked to a variety of other highly dangerous conditions such as heart disease, stroke, cancer, Alzheimer’s disease, and others. Unlike type I diabetes which is based on biological and genetic factors, type II diabetes is more associated with behavior and nutrition, although genetics and environmental factors play a role. More than 90% of diabetes mellitus cases are caused by insulin resistance that forms as a result of overweight/obese body composition ad inactive lifestyle. Evidence suggests that in most cases unhealthy weight is caused by nutritional disbalance and inappropriate eating habits. Therefore, drawing connections, the purpose of this research is to investigate the impact of nutrition on the development of Type II diabetes mellitus.
The disease is extremely widespread, affecting more than a third of the population, and being the 7th leading cause of death due to various stemming health complications. This has led to many experts in medicine and public health to dub diabetes and the associated obesity as an “epidemic” and “crisis” (Tavernise, 2015). The prevalence and seriousness of the disease is why this topic is critical to research and discuss. The nature of the condition is that it does not manifest physically until much later through diabetes-related retinopathy, neuropathy, heart disease, or kidney disease, all of which are interrelated (CDC, 2019) However, as soon as a patient reaches of a ‘prediabetic’ status, the metabolic changes are beginning to have an accumulating effect that later has a destructive effect that is much more difficult if at all possible to address medically. Diabetes mellitus in every sense of the phrase is a ‘silent killer’ which makes it absolutely critical to recognize and identify the disease early and proactively begin to manage or prevent it. Nutrition, accompanied by other lifestyle choices, is the primary factor in preventing or managing type II diabetes.
The research presented in this paper will benefit virtually everyone, ranging from individuals seeking to know more about Type II diabetes and how to prevent it, to medical professionals that may change their approach to treatment and recommending this as patient-education literature. Type II diabetes, or even the threat of it, is a widespread disease, and more people should become aware of it to stop the epidemic of this non-infectious condition. Recognizing the impact of nutrition on diabetes goes beyond personal choices, it is a national problem which affects virtually everyone. Therefore, anyone ranging from businesses in the food industry, institutions providing food to people at any given time (such as schools) to policymakers can benefit from the information to direct their course of action in preventive measures. The goal of this paper is to research relevant and clinically accurate information regarding the impact of nutrition on development of Type II diabetes and present the information in a comprehensive manner to be utilized in a variety of contexts which can help to prevent or treat the disease.
General Information
Diabetes mellitus, also known as Type II diabetes, is a chronic metabolic disease which affects the production and use of insulin in the body facilitating the uptake of glucose (blood sugar). Type II diabetes occurs when β-cells are unable to produce sufficient insulin to keep up with demand, characterized by insulin resistance. Insulin resistance develops with ectopic fat presence in the liver and muscle, as well as accumulating in the pancreas which leads to the decline of β-cells functionality and eventual death. Therefore, obesity is the major and primary risk for type-2 diabetes in combination with complex genetic and environmental etiology. Factors for onset type-2 diabetes may differ between individuals and race/ethnicity, as there are different, personal ectopic fat ‘thresholds’ at which insulin resistance and β-cells deterioration occurs. Insulin sensitivity decreases with obesity and increases with weight loss, making prediabetes or early onset Type II diabetes potentially reversible (Skyler et al., 2017).
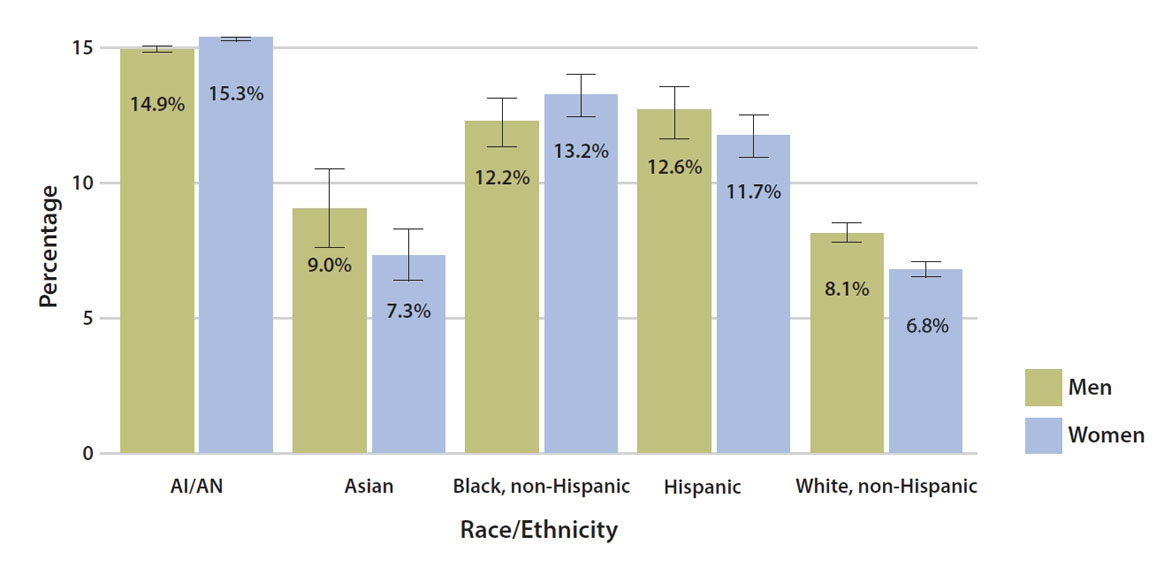
Traditionally, type 2 diabetes has been present in individuals of older age, but in recent years, there has been an increased incidence in youth. Approximately 210,000 Americans under the age of 20 are diagnosed with diabetes, or about 0.25% of that age group. Older age is correlated with risk of developing diabetes as one in four Americans over the age of 65 is diagnosed, or 26.8% (American Diabetes Association, 2020). Certain racial and ethnic groups such as African Americans, Hispanics/Latinos, Asians, and American Indians are more prone to developing the condition due to a mixture of genetic factors, lifestyle, and culture. Males are slightly more affected by Type 2 diabetes with 6.9% prevalence in comparison to 5.9% for females (Skyler et al. 2017). Geographically, the disease has significant variance, with South-East Asia and Australia having the most diagnosed adults of over 153 million, while North and Latin America have the highest incidence rates of 1 in 8 adults affected. Low socioeconomic status such as low education, low occupation, and low income can increase the risk of developing type II diabetes by 30-41% (Skyler et al., 2017).
Due to the extensive prevalence and health impacts of diabetes mellitus, there is an inherent socioeconomic burden. The estimated cost of diagnosed diabetes for the United States in 2017 was estimated at $327 billion, $237 billion of which were direct medical costs and $90 billion in reduced productivity. Based on cost category analysis, diabetes accounts for 1 in 4 health dollars spent in the U.S., with $16,750 annual average medical expenditures per patient with diabetes (American Diabetes Association, 2018).
The etiology of type 2 diabetes mellitus is complex despite being such a common disease. It is associated with a variety of irreversible risk factors such as age, race, and genetics, but also strongly correlates with controllable and reversible activities such as diet, exercises, and behaviors the likes of smoking and alcohol use. Therefore, while nutrition is not the only contributing factor – alongside physical activity, diet is regarded as the major impactful factor for development of type 2 diabetes around the world. Research has consistently identified a positive correlation between high intake of sugars such as carbonated drinks and added sugars popular in modern urban and developed societies and development of diabetes mellitus. Less consistent data but still important is the correlation between consumption of fats and carbohydrates in developing diabetes (Sami et al., 2017). As discussed earlier, obesity and ectopic fat deposits contribute to insulin resistance and hypoglycemia which define type 2 diabetes. Food intake is directly linked to obesity, both in volume of food as well as the composition and quality of the diet. Dietary compositions consisting of high intake of red mead, sugar, and fried foods result in an increased risk of insulin resistance and type 2 diabetes (Panagiotakos et al., 2005). Therefore, nutrition plays a highly critical role in the development and subsequent management of type 2 diabetes in order to regulate blood glucose levels and weight management to improve quality of life.
Application
The primary audience for this research are individuals who have been diagnosed with type 2 diabetes or have clinically recognizable prediabetes – both groups have the opportunity to modify nutritional and dietary habits in order to prevent, manage, or potentially reverse the condition. A significant challenge for stakeholders such as clinicians, is that the among patients, diabetes awareness is commonly very low. This applies to all populations, but some groups such as lower socioeconomic status, minorities, or elderly individuals may have very little understanding about the disease. Knowledge on the topic is critical to achieve better compliance with medically prescribed therapy, including changes to lifestyle and diet management (Sami et al., 2017). Meanwhile, a study by Magurova et al. (2012) found that providing diabetes education to patients increases the awareness of the disease and notably improves quality of life. Therefore, the research has significant applicability in clinical practice as a tool for patient education and awareness that improves adherence and dietary changes.
However, the unusual high prevalence for a non-communicable disease and rapidly growing rates of prevalence, particularly in populations that are typically health indicate that diabetes mellitus is a public health concern. It is an issue that should be addressed quickly as many public health experts deem to be a public health emergency that is on par to reach 642 million cases globally by 2040 and place a heavy burden on society and health systems (Al-Lawati, 2017). Everyone that is at risk of developing type 2 diabetes or has been diagnosed should shift priority to nutritional management due to its impact on the disease which is, as noted, progressive in its effects on human health. Meanwhile, the public health concern has prompted most developed countries to set national goals in reducing the burden of diabetes mellitus and improve quality of life and care for those who are diagnosed or at risk. This includes the United States, with objectives under its Healthy People 2020 initiative to reduce annual number of new cases, mortality, and control of symptoms for those who are diagnosed (HealthyPeople2020, n.d.). The importance of this topic is largely due to the critical nature of the growing incidence rates of diabetes mellitus, including in developing countries, vulnerable communities, and younger ages being affected. If left poorly managed, over time, this will translate into extreme burdens for society with overextended health systems, extreme medical costs, and socio-economic consequences (Tabish, 2007).
The topic of nutrition comes into play because the epidemiological and demographic patterns seen with type 2 diabetes are a consequence of social norms and behaviors in dietary habits. The rise in popularity of fast foods, added sugar, and other products have led to the epidemic of obesity or unregulated glucose, eventually inciting hypoglycemic individuals with type 2 or prediabetes diagnoses. High quality, fresh, and healthful diets are hard for many people to obtain, particularly in non-affluent areas (the concept known as food deserts where communities lack access to fresh foods, provided only with options of prepackaged and processed foods) (Sklaroff, 2012). At the macrolevel, the rising rates of the disease are attributed to a range of factors including urbanization, computerization, and shifts in food production that focus on longevity and processing of foods in order to be safely distributed along extended supply chains. At the same time, this has led to increased accessibility to unhealthy foods, further exacerbated by the franchising business models that led to emergence of fast food restaurants combined with cultural dietary preferences to promote high calorie content in large portion sizes (Let et al., 2014). Type 2 diabetes may be a personal health struggle, but it is a societal issue that is driven in part strongly by the status quo of promoted dietary practice in modern American culture.
Approaches/Treatments
The approach to management/prevention and treatment of type 2 diabetes requires examination of both the factors of nutritional strategies at the individual patient level and then a more comprehensive public health and policy levels. Decades of research on diabetes mellitus found the fundamental importance of individual nutrients and dietary patterns in the prevention and management of the disease. Similarly, just like the cause of type 2 diabetes, it is not single food items but rather application of food pattern techniques that ultimately result in the biological response and health results in prevention or treatment of the condition. Diets which are rich in fruits, vegetables, legumes, and wholegrains while moderating red meat, sugar, and alcohol consumption are associated with improving glycemic control and blood lipids. Diets such as Mediterranean, vegan, DASH, and others can be tailored to personal and cultural preferences to achieve the necessary results. When utilizing nutrition in the treatment of diabetes mellitus, it is vital to consider that quality of nutrients such as dietary fats and carbohydrates is more critical than quantity, and diets with appropriate calories needs for weight control will have successful impact on diabetes prevention or management (Let et al., 2014).
Public health interventions using the principle of glycemic risk stratification which targets high risk individuals (obese and presence of impaired glucose tolerance) are generally effective. The primary approach for public health is to prevent or mitigate modifiable risk factors in the population such as dietary habits, weight loss, and physical activity. Various examples of public health initiatives take the research basis mentioned in this paper regarding nutrition, dietary pattern structuring, and physical activity to achieve targeted outcomes. Public health programs are typically community-based with oversight and sponsorship form the government, health organizations, and local healthcare institutions. In the context of modern-day technology and the ongoing COVID-19 pandemic, delivery of programs for lifestyle change has been done online via telehealth and other Internet-based services to effectively reach more people. Public health programs, especially ones which are targeted, well-developed, and supported long-term have a moderate success rate of achieving 4-10% weight loss and improving dietary habits for high-risk individuals (Gruss et al., 2019). The evidence clearly suggests that lifestyle interventions, focused on nutrition and dietary patterns alongside physical activity are effective in preventing and delaying type 2 diabetes while being cost-effective in real-world contexts.
However, the long term economic, social, and personal consequences of type 2 diabetes make a viable case to have measures become policies aimed at prevention of disease incidence rates. Policies should focus on four primary aspects. First, there should be nationwide promotion and evaluation of healthy lifestyle programs, such as ones described above with a focus on prevention and treatment of obesity as well as nutritional guidance and active lifestyle. This is the responsibility of the public health sector aimed at translating evidence-based findings into practical and accessible programs. Second, health agencies should aim for early identification of subjects at risk of developing type 2 diabetes, including screenings for gestational diabetes, BMI, and other contributing factors in order to begin clinical interventions. (Steyn et al., 2004). Third, policy should aim at creating healthy products alongside the agricultural sector and private sector companies to shift the food practices in production that contribute to widespread popularity of prepackaged meals. Finally, policy should be targeted with legislative action at macro factors discussed earlier, such as regulation of food industry, improving access to healthy foods in impoverished communities, and general national efforts at reducing rates of obesity and improving dietary patterns and habits (Bergman et al., 2012). From a policy perspective approach, it requires the cohesive collaboration of three sectors – clinical, public health, and government regulation alongside the private sector in order to create effective programs and synergies to address the prevention of type 2 diabetes on a macro level.
Expected Outcomes/Recommendations
This section will focus on two expected outcomes, individual and from a public health perspective if appropriate measures are taken in improving nutritional intake and dietary patterns. For an individual patient, the expected outcome as a result of treatment and lifestyle changes is a combination of weight loss and lowering of glucose levels. Weight loss is measured via several tests including standard weight in, BMI, and a body composition test. The target is 7% of body weight loss in a year and those with impaired glucose tolerance, to reach HbA1c of <6%, preferably under 5.6% for normal indicators (Wilding, 2014). Such outcomes are realistic and possible in combination of diet for glycemic control alongside recommended 150 minutes of physical activity per week. Patients adhering to said lifestyle changes report significant improvements in glycemic index and weight loss, an indicator of increased insulin sensitivity and a remission/prevention of type 2 diabetes.
The key objective and data point from a public health perspective is to reduce the annual number of newly diagnosed cases of type 2 diabetes mellitus. This is the primary objective for the Healthy People 2020 initiative in the United States, which had set a 10% improvement goal for a 10-year period and had exceeded it going from baseline 8 cases per 1000 to 6.5 per 1000. The expected outcome is that further decrease is possible, with the objective to reach 5 cases per 1000 by 2030 (Healthy People, 2020). There have been significant improvements in public health awareness in the U.S. population, and a perceived change in dietary patterns towards healthier alternatives and diets. Many fast food and dining locations have also begun offering fresh and healthy options in light of population dietary changes and demands, gradually shifting the country away from the fast-food culture (Poinski, 2020). There is still significant progress to be made, and problems experienced by lower socioeconomic classes in terms of access to food are not fully resolved. However, the general popular trends are valuing a significantly healthier nutritional choices which has a long-term impact on type 2 diabetes prevalence.
The primary recommendation is for public healthy policy to continue strong measures in targeting underlying factors which impact the nutritional intake of Americans. This ranges from public education about nutrition and diabetes to policies which further regulate food industry and begin to reduce the levels of added sugar content particularly in non-sweet foods. Other elements which have had success such as legally reducing portion sizes and promoting healthy lifestyle interventions are valuable from a massive public health perspective. The ongoing COVID-19 pandemic has critically hindered the possibility of the overburdened healthcare sector to help patients with chronic conditions effectively. However, the pandemic also made many people to consider their health and wellness, which provides ample opportunities for public health and government to step in with appropriate guidance and information.
Conclusion/Summary
Type 2 diabetes mellitus is a serious metabolic disease which is characterized by insulin resistance and wrought with negative complications for short- and long-term health. The disease is caused by a wide range of genetic, environmental, and behavioral factors, but the majority of cases are associated with overweight and obesity. The disease is becoming prevalent around the world, impacting virtually all populations, including typically healthy individuals such as young people, which creates significant concern for the health burden of the disease in the population. This paper discusses the importance of nutrition in managing or preventing type 2 diabetes, examining all perspectives ranging from individual patients to public health and policy. The underlying cause of higher weight causing type 2 diabetes is a consequence of modern-day lifestyles which emphasize lack of physical activity and inappropriate nutrition. Addressing this issue through patient treatment and public health programs and policy has shown and will have further potential in improving dietary habits in the population and reducing incidence of type 2 diabetes.
References
Al-Lawati J. A. (2017). Diabetes Mellitus: A local and global public health emergency! Oman Medical Journal, 32(3), 177–179. Web.
American Diabetes Association. (2018). Economic costs of diabetes in the U.S. in 2017. Diabetes Care, 41(5), 917–928.
American Diabetes Association. (2020). Statistics about diabetes.
Bergman, M., Buysschaert, M., Schwarz, P. E., Albright, A., Narayan, K. V., & Yach, D. (2012). Diabetes prevention: global health policy and perspectives from the ground. Diabetes management (London, England), 2(4), 309–321. Web.
CDC. (2017). New CDC report: More than 100 million Americans have diabetes or prediabetes. Web.
CDC. (2019). Put the brakes on diabetes complications. Web.
HealthyPeople2020. (n.d.). Diabetes.
Gruss, S. M., Nhim, K., Gregg, E., Bell, M., Luman, E., & Albright, A. (2019). Public health approaches to type 2 diabetes prevention: the US national diabetes prevention program and beyond. Current Diabetes Reports, 19(9).
Ley, S. H., Hamdy, O., Mohan, V., & Hu, F. B. (2014). Prevention and management of type 2 diabetes: dietary components and nutritional strategies. The Lancet, 383(9933), 1999–2007.
Magurova, D., Majernikova, L., Hloch, S., Tozan, H., & Goztepe, K. (2012). Knowledge of diabetes in patients with type 2 diabetes on insulin therapy from eastern Slovakia. Web.
Panagiotakos, D. B., Tzima, N., Pitsavos, C., Chrysohoou, C., Papakonstantinou, E., Zampelas, A., & Stefanadis, C. (2005). The relationship between dietary habits, blood glucose and insulin levels among people without cardiovascular disease and type 2 diabetes; The ATTICA study. The Review of Diabetic Studies, 2(4), 208–208.
Poinski, M. (2020). Consumer trends shifting toward health and wellness, ADM finds. Web.
Sami, W., Ansari, T., Butt, N. S., & Hamid, M. (2017). Effect of diet on type 2 diabetes mellitus: A review. International Journal of Health Sciences, 11(2), 65–71.
Sklaroff, S. (2012). Diabetes affects millions; Society should not stigmatize its victims. The Washington Post. Web.
Skyler, J. S., Bakris, G. L., Bonifacio, E., Darsow, T., Eckel, R. H., Groop, L., Groop, P.-H., Handelsman, Y., Insel, R. A., Mathieu, C., McElvaine, A. T., Palmer, J. P., Pugliese, A., Schatz, D. A., Sosenko, J. M., Wilding, J. P. H., & Ratner, R. E. (2017). Differentiation of Diabetes by pathophysiology, natural history, and prognosis. Diabetes, 66(2), 241–255. Web.
Steyn, N., Mann, J., Bennett, P., Temple, N., Zimmet, P., Tuomilehto, J., Lindström, J., & Louheranta, A. (2004). Diet, nutrition and the prevention of type 2 diabetes. Public Health Nutrition, 7(1a), 147–165.
Tabish S. A. (2007). Is diabetes becoming the biggest epidemic of the twenty-first century? International Journal of Health Sciences, 1(2), 5-8. Web.
Tavernise, S. (2015). Global diabetes rates are rising as obesity spreads. The New York Times.
Wilding J. P. (2014). The importance of weight management in type 2 diabetes mellitus. International Journal of Clinical Practice, 68(6), 682–691. Web.