The purpose of this assessment is to evaluate the effect of parenting styles on decisions and children’s behavior. In particular, it focuses on difficulties such as the maltreatment of children and families at risk as well as the treatments that may be used to address them. To that end, the author has interviewed a family that consists of a single mother and a young daughter, to which they had no prior relationship. Based on the results, they developed therapeutic goals and determined the techniques that would yield superior results in addressing the problem. The family was informed about the purpose of the interview and briefed on confidentiality, and the author obtained their consent. All of the family information, including names and identifying characteristics, has been obfuscated to protect their privacy. Overall, the author has been able to find some problems and potential solutions for them, which will be presented below.
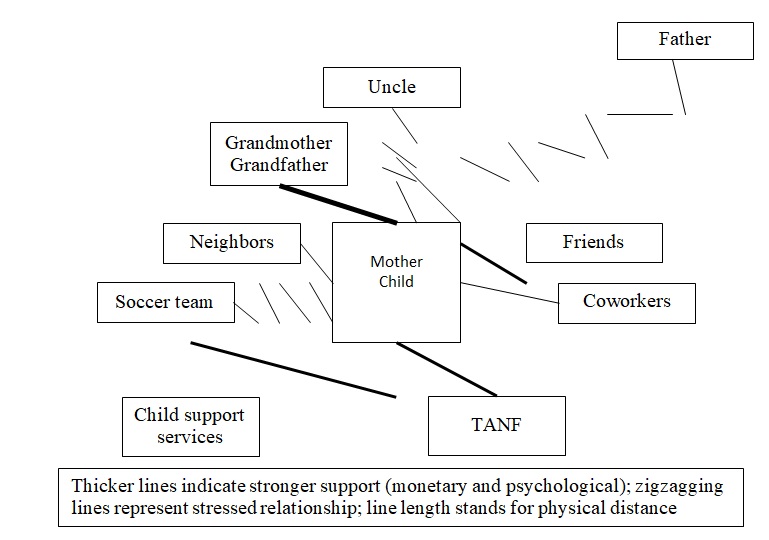
Family Map
Psychosocial Assessment
The family consists of two people: a mother (who will be named Mary for confidentiality purposes) and a son (named Chris for the same reasons). Mary is in the late twenties, while Chris is between five and ten years old. The father, Dave, left and moved away while Mary was still pregnant, severing all contact and refusing to acknowledge or help the child. Mary is Chris’s legal guardian, and her status as such has not come into question at any point. The two live in a moderately large city, renting a small apartment near the outskirts. Mary works part-time as a waitress at a restaurant, and she also receives aid from several government agencies. Still, the family frequently experiences financial issues, as the income that Mary can generate is not sufficient.
Medical aid is one of the areas in which the family struggles, as it often cannot afford out-of-pocket costs. The two use Medicare, though they may not be taking advantage of all of its coverage. Their PCP is a family doctor, whom they visit when Mary or Chris experience significant symptoms. Mary will often ignore her condition if it is not severe enough, but she will take Chris to see a medical professional whenever he shows signs of an illness. Sometimes, the family will also visit a pediatrician, but generally, Mary chooses the family doctor because it is more convenient to see them. The family has never visited either a psychologist or a psychiatrist, as Mary believes that there has not been a reason to suspect mental problems that would require their involvement. She claims that checking in with them without a significant cause would be too time-consuming and expensive, which is why she has not considered doing so.
Mary has some health problems, but she is trying to manage them with alternative medicine and personal observation as opposed to medical advice. She claims that her sight gets worse when she has been stressed for an extended period, which she tries to manage by avoiding pressure. She also complains about pain in her legs and lower abdomen, both of which happen intermittently and without an obvious trigger. Mary is choosing to ignore these problems until they make it challenging for her to do her job, believing that such a time will not come and the pains will pass. Chris seems to be healthy on the surface, being moderately physically active and not complaining about anything at the moment. With that said, he also does not receive medical checkups often, mostly visiting doctors when sick with the flu or other infections.
Mary and Chris live in the apartment alone, and people tend not to visit often. At times, Mary starts relationships with men, but these tend to be short-lived, and her boyfriends do not stay at the apartment. With that said, some, especially those whose relationship has gone on longer, used to visit frequently and interact with Chris. He responds to attempts at conversation with hostility, overtly expressing his dislike and crying at times. In general, Chris is prone to emotional outbursts and tantrums, though most of the time, he is quiet and reserved, preferring to play with his phone or go outside to meet friends. Mary thinks that the behavior is troubling and has stopped bringing people home to avoid aggravating Chris. With that said, she does not know what else she can do to address the situation and is presently waiting for her son to “grow out of it.”
Mary thinks that she and Chris are eating enough to stay reasonably healthy and fit without starving or gaining unnecessary weight. However, she admits that the diet she and her son are consuming is rather monotonous and limited. In particular, it is heavy on carb-rich products such as rice or pasta and lacks non-processed meats and vegetables. Mary claims that she often cannot afford the former because meat is too expensive and does not keep well. She also does not feed Chris many of the latter because he dislikes many vegetables and refuses to finish them. The child has not shown any overt symptoms of vitamin deficiencies yet, and the mother’s issues may have come from a variety of factors. However, Chris may be slightly too thin for his age from the author’s observation.
Mary does not get enough sleep as a result of having to work and care for Chris. Her shifts at the restaurant where she works are irregular in starting time and length, sometimes starting early in the mornings or ending at night. Whenever Mary has free time, she has to cook, clean, shop, and care for Chris, all of which take up a substantial portion of this remaining period. As such, Mary tries to sleep whenever she can, but generally, she claims that she cannot get eight hours of sleep every day. Chris has a more normal schedule, being active during the daytime and going to sleep at night. He does not appear to have any sleeping issues, while Mary generally reports exhaustion throughout the day.
Chris attends primary school, though this report will avoid listing the specific grade to obscure his age. He performs moderately well, neither achieving outstanding successes nor failing in ways that draw the teachers’ attention. Chris prefers mathematics and music lessons and performs well in them. He also dislikes handwriting and language arts, claiming that they are repetitive and dull. He does not attend Special Ed classes, as he does not have any disorders or disabilities that would qualify him for such. At times, Chris acts aggressively in school and fights other children, and Mary has been made aware of the problem. He has missed some days due to illness, but he has not skipped school willfully without a valid reason. While he may have some behavioral issues, the teachers have elected to ignore them for now and expect them to pass. As such, no prior testing or treatment for Chris’s behavior has taken place, as the behavior is seen as normal and temporary.
Mary has some friends with whom she goes out occasionally to relax and enjoy herself. Chris is also friendly with some local children and plays with them frequently, sometimes visiting each other. The two also frequently visit Mary’s parents, who support the family substantially and try to help with some needs. With that said, neither of the two are particularly close with their neighbors, generally staying home and communicating with others little when there. As mentioned above, Mary has had multiple boyfriends in the past, though she does not currently have one. These relationships tend to be short, and she claims that the men are unwilling to commit to a partnership with a single mother. Mary adds that her status as one has caused her social issues in general, as it influences the views of many people who learn of the fact negatively. She also recalls Chris’s complaints about being harassed by his classmates over not having a father, which is a sensitive topic for the child.
Mary has reported feeling substantial stress and anxiety as a result of the year’s events. The family’s already-tenuous financial status was further complicated by the COVID-19 pandemic, which has led her to lose her job as a result of the restaurant’s lockdown-related closure. The location has since been permitted to open, and Mary was able to return to her duties, but the intermediate period was troubling for her. The broader lockdown and self-isolation measures have also had an impact on the family, and Mary reports feeling stressed and anxious. She reports uncertainty over her future and concerns over the possible return of lockdown measures and the associated damage to her financial well-being. She claims not to have noticed any particular changes in Chris’s behavior over the period, though she also admits that she may not have been paying sufficient attention.
Mary does not play sports or engage in dedicated exercise, claiming that she has neither the time nor the energy to spend outside of her primary activities. Her hobbies usually involve passive ways to spend time, such as watching television, though she will sometimes go out with friends or take Chris somewhere. Mary is not religious and does not attend a church, and Chris follows her example. She does not smoke or use drugs, but she drinks in amounts she describes as moderate daily and occasionally engages in heavier drinking, mostly when with friends. Chris plays soccer, though his belligerence has led the coach to contact Mary and warn her that he may have to take her child off of the team. He is also active physically when he plays outside with friends, and overall, there are few reasons to be concerned about his fitness.
Mary has not expressed interest in counseling for the sake of improving her family situation, as she believes that the issues are not significant enough to require it. She says that she may consider engaging in the practice if it is a requirement for qualifying for some form of other aid, similar to how she has to work part-time to qualify for TANF. However, she refuses to pay for counseling or partake in it for free without other considerations, saying that she does not have enough time to justify spending it in this manner. Mary is more interested in the concept of a support group, especially one that meets online and does not require a dedicated time investment. However, she is skeptical about the benefits, claiming that her child is too old for her to apply much of the advice she is probably going to see.
Therapeutic Goals
Chris has not undergone prior evaluations for his issues, and so, it is not possible to say confidently whether he has any issues that require intervention. However, he has displayed a pattern of aggressive behavior, both in school and on the soccer team. So far, the school has not taken substantial action, but the team’s coach has already threatened to remove Chris from the team. This issue fits at least one of the criteria, namely aggression, for conduct disorder as defined by Martel (2018), with the other three being the destruction of property, deceitfulness or theft, and serious rule violations. It should also be noted that Mary does not appear to monitor her child closely, and, therefore, the other symptoms may manifest without her knowledge. A more thorough analysis is needed for Chris, but for now, the paper will proceed to assume a mild case of conduct disorder.
Conduct disorder is associated with automatic responses to stressors as a result of a variety of possible influences. As such, per Vanzin and Mauri (2019), therapy for it should aim to “lead the patient to relinquish automatisms in favor of behaviors, chosen by the patient herself, functional to the accomplishment of personal goals” (p. 43). With that said, this goal is overly general and should be adapted to Chris’s specific needs. He currently has a problem regarding aggression, and, consequently, that is what the therapy will try to address. The current goal for the therapy will involve teaching Chris alternate solutions for his emotions and various situations where he typically resorts to violence. To that end, it will aim to reduce the number of the child’s violent outbursts or eliminate them within the next six months.
Interventions to Be Used
Chris’s condition is a result of a number of different factors, both within the family and outside of its boundaries. Such a situation is standard for conduct disorder, and evidence-based practice has evolved to incorporate this fact. As such, Theodore (2016) recommends multisystemic therapy as the best-researched and most often recommended treatment for the issue. It is a combination of a number of different interventions that involve the family, the home, and the community. By involving all of these spheres, it aims to encapsulate the causes and effects of the issue, alleviating the former to prevent the latter from emerging. In this case, the school that Chris attends and his soccer team will have to be contacted, as their cooperation is required to ensure that the treatment is effective.
To understand the situation better, it will be necessary to document Chris’s behavior in more detail and analyze the altercations in which he gets and the undesirable acts in which he engages. To that end, the school and the team will be asked to monitor Chris’s behavior more closely and report any problematic events. Mary will also be asked to pay more attention to her child and his actions. Having obtained the required information and understood Chris’s character and responses to stressors better, a qualified therapist can discuss these problems with him and help him overcome his automatic reflexes. As Theodore (2016) notes, contact should take place several times a week in an environment that is the most comfortable for the child. With that said, personal interventions alone will not change the underlying factors of the problem, which need to be addressed for the improvement to be permanent.
Chris’s conduct disorder was able to advance without substantial interference due to Mary’s lack of oversight and general inattentiveness to her child. To address similar problems in the future, the two will have to learn to work together and share their troubles. Rubin (2012) recommends parent-child interaction therapy (PCIT), an evidence-based family intervention that teaches parents the skills they need to take care of their children. They do so by learning new approaches theoretically in a study session and then applying them practically with their child, using guidance from the therapist who is watching from the side. At the end of this therapy, the parent will be competent to take care of most or all of the child’s needs, preventing them from displaying problematic behavioral tendencies. They will also have the opportunity to strengthen their relationship with the child and earn their trust, reducing the chance that the child will withhold important information from them.
Brief strategic family therapy may also be helpful to address Mary’s general failure to monitor and support Chris. Per Patterson et al. (2018), it aims to address maladaptive family interactions that contribute to behavior issues and reform them into more productive activities. Mary’s and Chris’s family interactions will be analyzed, and a qualified specialist will identify their strengths and weaknesses. The former will be highlighted and reinforced to build confidence, and the latter will be reformed through coaching sessions. With the skills provided by PCIT and the new family structure that forms as a result of the procedure, Chris’s future mental well-being can be secured. Ultimately, the combination of the three interventions should be adequate to both eliminate current symptoms and ensure that the family can handle future difficulties and prevent them from reemerging.
Practice Effectiveness Evaluation
For the purposes of assessing the effects of the intervention, the author will employ a pretest-posttest result. They expect to see a tangible change in Chris’s behavior, which will likely have both readily apparent and more obscure ramifications. In particular, his violent outbursts should become substantially less frequent or disappear altogether, which will need to be reflected in the results of the assessment. There are some concerns regarding the effectiveness of the approach given the extremely small size of the sample, but the same problem would apply to most other methods. As such, the pretest-posttest design is appropriate for roughly evaluating the effectiveness of the treatment, though it should not be taken as a highly reliable indication of success or failure.
The Conduct Disorder Scale will be used to evaluate Chris’s state and track changes in it as the treatment progresses. It consists of forty items that aim to evaluate the four categories of the condition’s definition, as described above. It also provides an interview form for issues that are infrequent but still significant and indicative of conduct disorder. According to Pierangelo and Giuliani (2018), it is the only test of its kind to provide standard scores for the identification of the condition. As such, it can be used to determine the severity of Chris’s issues with substantial precision. The test was chosen both for this quality and its provision of standard scores and percentiles that enable interpretation. Its findings can supplement the therapist’s expertise and provide a more comprehensive evaluation of Chris’s condition.
Along with the advantages listed above, the Conduct Disorder Scale is also distinguished by its evidence-based nature. As Pierangelo and Giuliani (2018) claim, it was standardized on 1,040 persons from a variety of groups, including people with conduct disorder and those with other similar conditions, and normalized based on 644 people who were afflicted with the issue. As a result of this effort, it can distinguish children with conduct disorder from those who are healthy but display behavioral issues and those who have other problems, though it may not necessarily be able to identify what additional issues they have. As such, if the area of focus is solely conduct disorder, as it is in this case, this test should be highly appropriate and useful, monitoring the child’s progress toward a healthy state.
However, this focus may also be seen as a disadvantage of the test, as it is unable to recognize other possible problems, even if it can hint at their existence. It is currently unclear whether Chris’s condition is conduct disorder or if it is his sole mental health issue. As such, once the situation is clarified, the therapies provided and the evaluation method may not prove as effective as necessary. In that case, substantial adjustments may be required, which are beyond the scope of this paper. Moreover, if Chris’s progress does not lead to recovery but only to the elimination of the conduct disorder, specifically, the test can miss the problem. With that said, all of these contingencies are challenging to avoid in any case, and in the current circumstances, the test seems the most relevant.
Conclusion
Overall, the low socioeconomic status of the family and the mother’s single-parent status have likely led her to pay inadequate attention to her child. Chris may also have been bullied or otherwise pressured at school, which would likely have a substantial effect on him due to his young age and the sensitive topic. As such, he may have developed a conduct disorder, which manifests in his aggressive and violent behavior at school and during games. With that said, a combination of multisystemic therapy, parent-child interaction therapy, and brief strategic family therapy should alleviate the condition and ensure that the family can prevent it from emerging again. The Conduct Disorder Scale may be used to monitor the decline in the problem’s prevalence in a pretest-posttest design. While it may not be adequate, a trained professional’s oversight should help direct the treatment and identify other potential issues.
References
Martel, M. M. (Ed.). (2018). Developmental pathways to disruptive, impulse-control, and conduct disorders. Elsevier Science.
Patterson, J., Edwards, T. M., & Williams, L. (2018). Clinician’s guide to research methods in family therapy: Foundations of evidence-based practice. Guilford Publications.
Pierangelo, R., & Giuliani, G. (2018). The special educator’s comprehensive guide to 301 diagnostic tests. Wiley.
Rubin, A. (Ed.). (2012). Programs and interventions for maltreated children and families at risk. Wiley.
Theodore, L. A. (Ed.). (2016). Handbook of evidence-based interventions for children and adolescents. Springer Publishing Company.
Vanzin, L., & Mauri, V. (2019). Understanding conduct disorder and oppositional-defiant disorder: A guide to symptoms, management and treatment. Taylor & Francis.