Statement of the Issue
The current policy brief describes the issue of oral and dental healthcare in the United States during the COVID-19 pandemic. It also addresses the challenges that dental offices currently experience when providing the clients with the services needed for maintaining an adequate level of oral health. As oral health has been linked with positive COVID-19 outcomes, the policy brief aims to examine and propose solutions for the issue of limited access to dental services during a pandemic for future implications.
Background
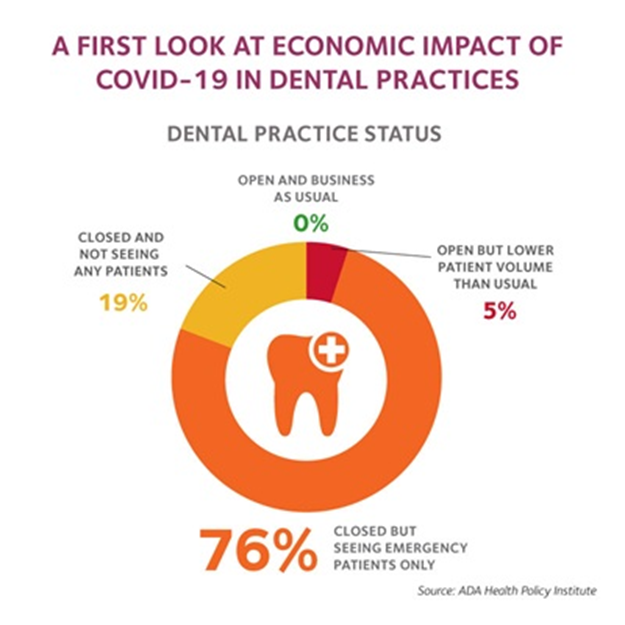
Oral hygiene is a pressing issue in the current COVID-19 pandemic due to numerous reasons. World Health Organization(WHO, 2020) showcases that the number of infected people in the U.S. continually rises, with more than 4,5 million confirmed cases to date (para. 1). According to the American Public Health Association (APHA, 2020), COVID-19 is a virus that is spread mainly by contact with the infected person’s respiratory secretion like saliva. As a result of the emergency protocols issued by the Centers for Disease Control and Prevention (CDC, 2020), dental services have been majorly shut down and restricted due to their high-risk ranking. According to the American Dental Association (ADA, 2020), currently, 76% of dental practitioners see only emergency patients, less than 20% are closed, and around 5% are open with lower volumes of patients (fig. 1). As seen from the pie chart, it is evident that no dental clinic operates as a usual, which poses an abundance of challenges for dental practitioners. Furthermore, the emergency leaves many patients in need of treatment unattended.
The main issue of the current dental services’ closure is its relation to oral health and increased risks of infection. The majority of severe COVID-19 cases are connected with vulnerable populations that are either older adults with weakened immune system or patients that suffer from hypertension, diabetes, heart disease, and so forth (APHA, 2020). However, while these patients substitute most of those infected, there is also a considerable portion of severe cases of COVID-19 among seemingly healthy and young individuals.
This inconsistency poses a question about the hidden factors that put the American population at risk. A study by Sampson, Kamona, and Sampson (2020) has shown that more than half of all infected patients die from the bacterial superinfections as a consequence of COVID-19 rather than from the virus itself. This finding concludes that “an increased risk of complications and death from COVID-19 are also associated with altered oral biofilms and periodontal disease” (Sampson et al., 2020, p.972). More than that, Shanti et al. (2020) also have found that lack of access to dental practitioners’ care will most likely lead to an increase in “oral potentially malignant disorders” like cancer (p. 1497). Therefore, post-viral complications are greatly associated with one’s oral hygiene and poor dental care or the absence of one can indirectly lead to severe medical consequences in the current epidemic, even for healthy people. Consequently, the ongoing closure of dental services poses risks for public health and should be reassessed in the framework of the COVID-19 emergency and for future implications.
Issues Pertinent to the Policy Brief
To examine the issue in more detail, it is essential to outline the additional information pertinent to the problem of dental care during the COVID-19 pandemic. As of August 2020, dental care is highly restricted by the CDC and is allowed to be conducted in emergency cases. According to the statement by CDC (2020), “all elective, nonessential medical, surgical, and dental procedures be delayed during the coronavirus outbreak” (para. 15). This law ensures that dental services, which are highly subjected to be a source of infection spread due to contact with patents’ respiratory secretions, are not posing a risk for public safety. However, more dental clinics reopen and return to their regular functioning in some states due to the decrease in COVID-19 influence.
In light of the aforementioned regulations and laws concerning dental services, many dental clinics have experienced some challenges and adapted to the current climate. More specifically, dental medical staff have adopted a dress code of protective wear. If a patient displays symptoms of COVID-19, they are strongly advised to seek medical assistance (CDC, 2020). If a staff member gets infected, strict screening and isolation techniques are utilized. The current state of dental services has also given a rise to a debate about the necessity of distance diagnosing and treatment options that have been widely inaccessible in public dental care. While medical clinics are examining emergency cases, patients with less urgent issues suffer from the inability to seek treatment.
While the current state of dental healthcare is aimed at minimizing COVID-19 cases, the results are mixed. CDC (2020) stated that reducing the number of patients in clinics does not necessarily lead to lessening the chances of infection. Furthermore, the risks currently experienced by the medical staff are widely mediated by emergency procedures like protective wear. On the other hand, there is growing evidence that lack of dental hygiene is one of the sources of COVID-19. For instance, access to dental healthcare is greatly reduced for the elderly who constitute the demographic endangered by the viral infections perpetuated by the neglect of dental conditions. The neglect leads to worsening their overall health and possibly contracting COVID-19. The same applies to people with disabilities who, under normal circumstances, are more vulnerable to infections and have decreased access to dental hygiene and applicable services.
Lastly, the fact that oral hygiene helps to avoid and identify COVID-19 on the early stages of being infected clashes with the current legislative framework. Policy limitations stop people from maintaining and improving their overall oral health, which has been proven to aid a person’s overall well-being (Ren, Rasubala, Malmstrom, & Eliav, 2020).On the contrary, neglect of one’s oral health is associated with a higher chance of developing respiratory infections. Given this data into consideration, Sampson et al. (2020) have shown that the neglect of oral health provoked by the limitations of the COVID-19 lockdown has indirectly increased the vulnerability of many people. Furthermore, “oral health researchers may play a more active role in early identification and diagnosis through deciphering the mechanisms of dry mouth and taste loss in patients with COVID-19” (Ren et al., 2020, p. 202). Therefore, the lack of oral health maintenance and virus identification in dental clinics does not allow for effective virus containment and prevention.
Response and Policy Options
Several governmental institutions and agencies have responded to the issues of dental care during the COVID-19 pandemic. The longevity of the lockdown has created a pressing urgency for dental problems among the patient population. As a result, the U.S. Department of Health & Human Services issued a set of rules that regulate dental care in the pandemic’s climate (CDC, 2020). The main guidelines cover the requirements concerning dentists’ and nurses’ protective wear and regulations regarding two main types of patients: regular ones and those at risk of contracting COVID-19. As it concerns the protective gear, medical staff is obliged to wear an “N95 respirator or a respirator that offers an equivalent or higher level of protection during aerosol-generating procedures” (CDC, 2020, para. 4). In addition, they must wear protective glasses for eyes, nose, and mouth to avoid contact with “respiratory secretions during patient care encounters, including those where splashes and sprays are not anticipated” (CDC, 2020, para. 15). Upon examining the policy’s regulation of protective wear, it is safe to assume that the main focus is employee protection.
As it concerns allowing patient care, the policy limits dental visits only to emergency cases. When a doctor suspects that a patient might be a carrier of the virus, they should encourage them to seek help or contact 911 personally. Knowingly engaging in care for a COVID-19 patient requires an additional level of security and protective wear. The existing policy examination shows that current dental practices are safe but extremely limited to emergency cases, which significantly disfavors specific demographics and oversees an issue of the interrelation between poor dental hygiene and COVID-19.
Some of the policy options that have been proposed to the CDC by the policymakers and dental researchers include distancing dental care, allowing free dental cleaning, and grants for vulnerable populations. Firstly, online dental care with reimbursement is one of the opportunities in public healthcare that will allow many people to avoid emergency situations and maintain their oral health (Ren et al., 2020). Secondly, free dental cleaning as a practice for future implications is an opportunity to reduce the risks of potentially lethal patient outcomes. It will ensure the overall level of awareness about the need in oral health (Sampson et al., 2020). Granting vulnerable populations free dental care is a third policy option that is forecasted to protect older, low-income, and disabled people from the effects of viral infections.
Recommendations
This policy brief proposes introducing remote dental services, raising awareness of the necessity of oral health, and providing educational opportunities for people to maintain oral hygiene at home. Firstly, local hospitals and dental offices should be encouraged to implement and actively practice remote care as an alternative to in-person visits. Ren et al. (2020) stated that unlike other areas of healthcare, remote diagnosis and treatment had been suppressed in dental care in favor of a more traditional approach. However, in the climate that requires social distancing and maintaining oral health for reducing risks of viral infection, Internet sessions with dental professionals might be a key to safe patient outcomes. They will allow for a safe and risk-free interaction that will ensure that the patient gets the help and guidance needed to avoid their oral health being compromised during a pandemic.
Additionally, if no online consultations are available, patients should have access to readily available information about maintaining oral health. While not as effective as in-person sessions, this approach will minimize the risks of dental emergencies and encourage better oral care among high-risk patients (Ren et al., 2020). Local healthcare providers should distribute these educational materials both to the groups most targeted by the virus and regular citizens.
Lastly, an addition to the CDC policy that might mediate the effects of inaccessible healthcare during a pandemic can grant the most vulnerable populations a chance for diagnosis and treatment. As Shanti et al. (2020) proved, the risk of developing potentially lethal oral diseases rises as non-emergency oral health maintenance becomes non-priority for dental clinics. Therefore, providing access to these services during the non-emergency period is essential in mitigating risks and reducing the likelihood of the dental emergency to appear.
References
American Dental Association. (2020). The health policy institute: COVID-19. Web.
American Public Health Association. (2020). COVID-19. Web.
Centers for Disease Control and Prevention. (2020). Guidance for dental settings. Web.
Ren, Y., Rasubala, L., Malmstrom, H., & Eliav, E. (2020). Dental care and oral health under the clouds of COVID-19. JDR Clinical & Translational Research, 5(3), 202-210.
Sampson, V., Kamona, N., & Sampson, A. (2020). Could there be a link between oral hygiene and the severity of SARS-CoV-2 infections? British Dental Journal, 228(12), 971–975.
Shanti, R., Stoopler, E., Weinstein, G., Newman, J., Cannady, S., … Rajasekaran, K. (2020). Considerations in the evaluation and management of oral potentially malignant disorders during the COVID -19 pandemic. Head & Neck, 42(7), 1497-1502.
World Health Organization. (2020). United States of America: COVID-19. Web.