Abstract
In the contemporary health care setting, pressure ulcers pose a serious health risk for individuals who cannot move on their own. Pressure ulcers may lead to severe complications and highly adverse conditions, and in some cases–even to a lethal outcome. Therefore, it is paramount to develop methods for more effectual pressure ulcer prevention. Thus, the current paper proposes a study comparing two methods for preventing pressure ulcers: the pressure ulcer protocol and the standard care. Quantitative, correlational research is suggested. It is recommended to collect data from at least 133 participants randomly assigned to either an experimental or a control group about the stage of development of pressure ulcers on their body after three days since hospitalization has passed. It is advised to analyze the data using Pearson’s chi-square test to find out whether there were any statistically significant differences between the two approaches for pressure ulcer prevention. Based on the results of the proposed study, it will be possible to make conclusions about which of the two said pressure ulcer prevention methods is more efficacious.
Introduction
In the modern health care setting, pressure ulcers pose a considerable risk to patients who cannot move on their own. This condition often develops during a hospital stay and leads to highly adverse health outcomes. The current paper proposes a quantitative correlational study for comparing two methods for preventing pressure ulcers in the clinical setting: the standard care versus the pressure ulcer protocol. After providing the problem statement and a review of relevant literature, the paper contains a description of methods for studying the said problem and for analyzing the collected data. After that, the expected findings are discussed, and the conclusion is provided.
Problem Statement
Because pressure ulcers pose a significant health risk to stationary patients, the problem of finding out which methods for their prevention may be the most effectual is of paramount importance (Swafford, Culpepper, & Dunn, 2016). For the current project, it is proposed to investigate the following PICOT question: In patients who are faced with considerable risks of acquiring pressure ulcers (P), does the utilization of a pressure ulcer protocol in the emergency department (I) allow for lowering the rates of pressure ulcers developed in the hospital setting (O) on the third day after hospitalization (T) when compared to the provision of usual care (C)?
Review of Literature
According to the relevant scholarly literature, pressure ulcers develop when a patient is occupying the same position for a considerable amount of time (Mallah, Nassar, & Badr, 2015). This condition emerges when there exists an inadequate supply of blood to certain tissues due to pressure or pressure and friction (Edsberg et al., 2016). It develops gradually; according to the classical staging, at the first stage, the area of skin that is under pressure becomes affected by redness that does not blanch and may be thicker or of a different temperature than the surrounding skin (Jiang et al., 2014). At the second stage, a part of the dermis is lost, which results in thickness reduction of the affected area (Jiang et al., 2014). The area has the appearance of an open ulcer that is still not deep; however, it may appear as a blister filled with serum (it can be torn or intact). At the third stage, the full thickness of the tissue is lost; it may be possible to visually observe the subcutaneous fat tissue, but muscle, bone tissue, or sinews cannot be seen yet (Jiang et al., 2014). At the fourth stage, sinews, bones, and muscles may be exposed; slough is sometimes observed in the bed of the wound. Depending on which part of the body is affected, pressure ulcers may be of different depth (Edsberg et al., 2016).
On the whole, pressure ulcers pose a significant health risk to stationary patients (Mallah et al., 2015). This may include patients in intensive care units, individuals who have recently undergone surgical procedures, people of advanced age, and so on. In certain cases, pressure ulcers may lead to serious complications, sometimes causing even lethal outcomes (Goudie et al., 2015). Even though it is stated that during the period spanning from 2006 to 2015, the prevalence of pressure ulcers has significantly decreased (dropping from 13.5% in 2006 to 9.3% in 2015 overall in all facilities that were investigated during a study in the U.S.), it still affects a significant percentage of patients (VanGilder, Lachenbruch, Algrim-Boyle, & Meyer, 2017). Therefore, the literature indicates that it is pivotal to take further steps aimed at reducing the prevalence of pressure ulcers, in particular, by developing and testing methods for effectively lowering their rates (Swafford et al., 2016).
Methods
To carry out the proposed study, hospitalized patients admitted to the emergency department and faced with a risk of developing pressure ulcers, but having no pressure ulcers at the moment of admission, will be identified. These patients will be randomly assigned either to the experimental or the control group. The patients from the intervention group will be cared for using the pressure ulcer protocol. The patients from the control group will be provided with standard care. On the third day after hospitalization (that is, after nearly 72 hours have passed after the patient was hospitalized), the patients will be assessed to find out whether they have developed the pressure ulcers, and if yes, which stage of the pressure ulcer they have. This data will be collected for further analysis. For each case, the information about the group (experimental or control; the independent variable) and the stage of the pressure ulcer after approximately 72 hours of hospitalization (the dependent variable) will be recorded. It should be noted that the pressure ulcers will be assessed according to the following scale: 0 = no pressure ulcer, 1 through 4 = at the corresponding stage (1-4) of the development of a pressure ulcer (Jiang et al., 2014). Due to the peculiarities of the proposed analysis, it will be needed to use a sample of at least 133 participants (see below).
Data Analysis
First of all, all the collected data will be transformed into the digital format to conduct the analysis. To find out whether the type of intervention correlated with the development of ulcers, it will be required to utilize specialized statistical software, such as Microsoft Office Excel or IBM SPSS Statistics. Pearson’s chi-square test will be employed (Field, 2013). This test will allow for finding out whether there is a statistically significant association between the independent and the dependent variables (Field, 2013), and making conclusions about the relative effectiveness of the two methods for the prevention of pressure ulcers.
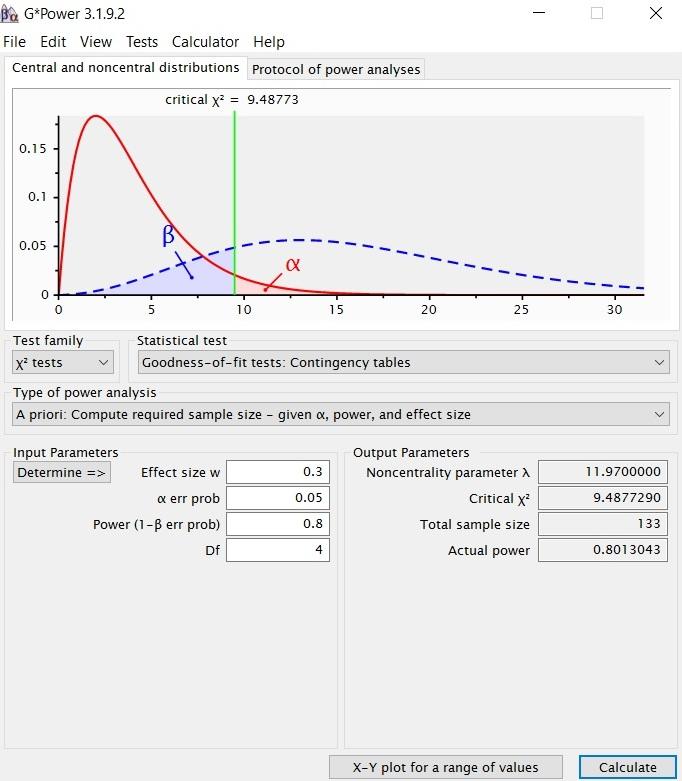
It should be noted that the standard level of statistical significance (α =.05) will be used in the test (Field, 2013). It will be expected to detect an effect whose size is at least medium (effect size w =.3). Because there will be 5 groups in the dependent variable, the degrees of freedom of the test will be 4 (Field, 2013). Also, it will be aimed to achieve at least the standard level of power of.80 (Field, 2013). From these parameters, it is easy to calculate the required sample size using the G*Power software (Heinrich Heine Universität Düsseldorf, n.d.). As can be seen from Figure 1 below, the minimal required sample size is 133 participants.
Discussion and Findings
After carrying out the Chi-square test, as discussed above, the researchers will make conclusions about the relative effectiveness or ineffectiveness of the pressure ulcer protocol in question when compared to the usual care. It is expected that the pressure ulcer protocol will be more effective than standard care. The findings will then be discussed further; it will be possible to propose the preferred method of caring for patients who are at risk of developing pressure ulcers. It will also be pivotal to discuss the limitations of the conducted analysis. Currently, it is possible to assume that the study will have some limitations related to the impact of possible confounding variables. In order to confirm the findings, further investigations of this problem will be needed.
Conclusion
All in all, pressure ulcers pose a considerable health risk for numerous patients who are unable to move on their own. The current paper proposes a study for investigating the comparative effectiveness of two methods of care for preventing pressure ulcers: the pressure ulcer protocol and the standard care. Based on the results of the study, conclusions will be made to decide which of the two methods is more effective to avoid the development of pressure ulcers in stationary patients.
References
Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing, 43(6), 585-597.
Field, A. (2013). Discovering statistics using IBM SPSS Statistics (4th ed.). Thousand Oaks, CA: SAGE Publications.
Goudie, A., Dynan, L., Brady, P. W., Fieldston, E., Brilli, R. J., & Walsh, K. E. (2015). Costs of venous thromboembolism, catheter-associated urinary tract infection, and pressure ulcer. Pediatrics, 136(3), 432-439.
Heinrich Heine Universität Düsseldorf. (n.d.). G*Power: Statistical power analyses for Windows and Mac. Web.
Jiang, Q., Li, X., Qu, X., Liu, Y., Zhang, L., Su, C.,…Wang, J. (2014). The incidence, risk factors and characteristics of pressure ulcers in hospitalized patients in China. International Journal of Clinical and Experimental Pathology, 7(5), 2587-2594.
Mallah, Z., Nassar, N., & Badr, L. K. (2015). The effectiveness of a pressure ulcer intervention program on the prevalence of hospital acquired pressure ulcers: Controlled before and after study. Applied Nursing Research, 28(2), 106-113.
Swafford, K., Culpepper, R., & Dunn, C. (2016). Use of a comprehensive program to reduce the incidence of hospital-acquired pressure ulcers in an intensive care unit. American Journal of Critical Care, 25(2), 152-155.
VanGilder, C., Lachenbruch, C., Algrim-Boyle, C., & Meyer, S. (2017). The International Pressure Ulcer Prevalence™ survey: 2006-2015A 10-year pressure injury prevalence and demographic trend analysis by care setting. Journal of Wound Ostomy & Continence Nursing, 44(1), 20-28.