Abstract
Opiate dependence is a growing problem in both young adults and patients who have developed addictions while receiving pain management regimens. The objective of treating patients with opiate addiction is to suppress withdrawal symptoms while facilitating the detoxification process. Buprenorphine-based regimens have gradually replaced methadone as the drug of choice for opioid dependence related to safety and increased access to care. Recent studies show that the efficacy of buprenorphine is equivalent to that of methadone when sufficiently high buprenorphine doses are prescribed in combination with rapid induction and flexible dosing.
This retrospective study reviewed data on 200 patients who were treated with buprenorphine for rapid detoxification at a medical center. Demographic information such age, employment status, type of opiate abused, number of years of drug abuse and physical characteristics of the patient were collected. Data were analyzed to determine the effectiveness of buprenorphine to reduce withdrawal symptoms commonly associated with opiate addiction such as, sweating, anxiety, tremor, nausea and pulse rate.
Introduction
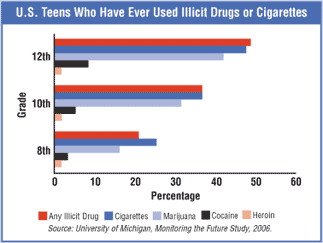
Opiates are becoming a major risk to the well being and health of humans in many societies with dramatic rise in drug dependence and reliance. Statistics show that more than 8% of the America population abuses opiates. American youth between 20 and 30 are the most affected with a reported incidence of fifty percent of drug abusers. In the past, the abuse of opiates was limited to youth between the ages of 13 and 30. However, recent studies report increased incidences of children below the ages of 13 being addicted to opiates as a common occurrence today. The use of opiates among the youth has been found to start between the ages of 10 to 13 with addiction established in the late teens. It has been found that half of all American twelfth-grade students have used an illicit drug at one time in their lives (World Health Organization, 2009.)
Opiates are defined as all drugs that contain opioid alkaloids, which when metabolized are responsible for producing dizzying and relaxing effects on individuals. Common examples of opiates in the United States (US) include morphine, heroin and hydrocodone. Abuse of these drugs among the youth is mainly through sniffing and smoking. These methods are used because of the belief that sniffing these drugs is less risky than injections. There have been more cases of drug overdose by abusers who inject opiates compared to those who smoke or sniff. The danger of injections is that failure to regulate the amount of drug that the user introduces into the body may result in serious damage to the user’s health (Millman, 2007).
The spread of opiate use in America has been promoted by the lack of proper education among the youth regarding opiate drugs and their effects. It is because of the misconceptions that youth have, that make the treatment and rehabilitation of opiate addiction difficult. There are common misconceptions about opiate abuse namely:
- If you sniff and smoke you will not become addicted
- Opiates are cool and if you abuse them you become cool too
- Opiates are good stress relievers
- If you can control it and use it once in a while, then the drug is good
These misconceptions were collected from the opinions of a random sample of American youth in grades eight to twelve. Such attitudes are what fuel the inception of new abusers and graduation of amateur abusers into serious addicts (World Health Organization, 2006).
Opiates are commonly used due to the effects that they bring to the user. They are also used in pharmaceutical prescriptions, but when prescribed- they are strictly used with care to avoid addiction. Once a person is addicted to opiates, it becomes a habit that is virtually impossible to quit. Opiates are used primarily to relieve pain, but cause various side effects namely nausea and vomiting, intoxication, stress / depression, coma and even death.
Treatment of Opiate Addiction
Continued abuse of opiates often leads to the destruction and damage of the central nervous system. Opiates hinder the production of endorphins by the brain and this leads to the degeneration of nervous tissue. This leads to death of brain cells and results in an inability of the brain to function properly. Continued use of opiates may lead to significantly reduced brain functionality. Nervous tissue also becomes dependent on the opiates for proper functioning, and it is this dependence that causes symptoms such shaking once the patient is withdrawn from opiates. It is important for all practitioners who are treating opiate addiction to understand how opiates work and how they affect the bodies of their patients in order to provide treatment effectively (Doweiko, 2006).
Psychological aspect of treatment
Healing and treatment begin in the mind. True healing can never be possible without healing the mind first. Many rehabilitation and treatment attempts that are carried out on people who abuse opiates fail because these addicts lack the mental and psychological motivation that is required to see them through the process. Treatment can only be said to be effective if it provides lasting solutions to the problems that the addicts face. If the process offers a temporary solution then it cannot be called a treatment success (Langrod, 2008).
Many patients relapse or revert to their old habits once they are out of the rehabilitation center or have completed their rehabilitation program. Mental healing has been found to provide more lasting solutions to the problems of people addicted to opiates. By healing the mind of an addict, the possibility of the addict to reverting to prior behaviors are reduced (Silk, 2009).
The first step in the psychological healing of an opiate-addicted person is for the addict to:
- Acknowledge that he/she has a serious and dangerous problem
- Acknowledge that he/she needs urgent treatment
- Acknowledge that he/she needs to take control of his/her condition
Most patients experience withdrawal symptoms which can lead to serious physical effects once opiates are discontinued. The literature confirmed several medications that suppress the effects of withdrawal (Maremmani, 2010). Psychological healing cannot work on its own and must be integrated with medication to facilitate proper physiological healing. If the patient fails to acknowledge the addiction, no treatment process will ever be effective. It has been reported that addicts that often heal themselves; not the practitioners, the detoxification drugs or the counselors which just facilitate the process. Therefore it is crucial for practitioners to integrate physical detoxification and psychological ‘healing’ in order to achieve the desired results and prevent relapse (Strain, 2005).
Dangers of rapid opiate detoxification
Rapid opiate detoxification (ROD) is on the rise and promises instant and immediate healing for patients addicted to opiates. ROD programs seem to be a definitive option to enable patients to overcome their addiction, but this is very far from true. This procedure is very harmful and has serious effects on its patients. ROD has been found to cause renal failure, heart failure and in some instances death. A New Jersey incident in which six patients on ROD died in a four-year span due to the procedure is just one example of the risks of ROD (Orman and Keating, 2009).
The effectiveness of rapid detoxification as a treatment for opiate addiction is still under question. Despite claims that after the procedure the patient becomes independent of opiates within 4 to 48 hours these methods are yet to be well tested. Some studies show that patients have withdrawal symptoms after 24 hours and that more than 80 percent of these patients often go back to the addiction after a six month period (Thakkar, 2008). These studies indicate that ROD is an ineffective method of opiate addiction treatment and that its effects do not justify its risks (Magnelli et al, 2010).
Traditional forms of detoxification are still the preferred and most reliable methods for treating opiate addiction. This is because these methods use agonist medicines that neutralize the effects of opiates on the patient’s body and minimize the effects of withdrawal. Traditional detoxification methods are more careful and procedural so that they minimize incidences of fatalities (Renner, 2009).
Conventional detoxification programs
Traditional methods of detoxification are controlled processes that entail the gradual detoxification of the patient’s body. During detoxification, the doses of drug intake by the patient are gradually reduced over a long period of time so as to avoid withdrawal symptoms. These traditional programs make use of drugs whose mode of action imitates opiates but does not have similar side effects to opiates. The drugs are administered in a structured manner so as to eliminate the patient’s dependence on opiates. After the patient has gained physical independence from opiates he/she is then taken for counseling to enable him / her to acquire psychological independence.
Buprenorphine
Buprenophine is an opioid-like heroin and other addictive drugs. However, it is widely used in detoxification processes as it aids in minimizing the effects of withdrawal. Buprenorphine does have negative effects on patients such as its ability to cause euphoria, but this is a compromise that is taken to ensure recovery and healing.
Buprenorphine is classified in the phenanthrene class, and is made up of a hydrocarbon that has been fused with benzene rings. It is a synthetic opioid but is not as strong as natural opioids such as morphine. It was approved in 2002, when its use was initiated in detoxification programs (Marquete, 2008).
Buprenorphine attaches itself to brain cells like natural opioids, binds more strongly than opioids and thus hinders natural opioids from reacting. Because of this binding ability, buprenophine has the capability to relieve the severe stress and depression that often accompanies opiate withdrawal (Courtwright, 2009).
Buprenorphine is favored as a method of reducing opiate addiction and dependence because it is a safe method that poses minimal threat to the user. When patients increase the intake of the drug its agonistic effects increase. Agonistic effects are directly proportional to the dosage, but with time the patient reaches a plateau phase when the agonistic effects do not increase (Kleber, 2008). This means that if a patient uses excessive amounts of buprenorphine it can never result in dizziness as is documented with heroin and morphine.
Buprenorphine has also been found to have a long half life that makes it possible for the detoxification of patients to be done with one dose every two to three days. This means that a patient could be withdrawal symptom free for up to 80 hours. Buprenorphine is available in a 30 day home kit that facilitates self administering the detoxification process. This drug is permitted by American legislation and patients can acquire required doses without the need for strict medical approval. Opiate addicts can acquire these drugs through licensed prescribers and conveniently self administer the treatment with medical supervision (Junig, 2009).
The most common methods of Buprenorphine administration are intravenous, intramuscular and sublingual. The preferred method to ease withdrawal symptoms is by rapid intravenous infusion which takes about three minutes to distribute the drug evenly into the blood stream and more than 48 hours to be eliminated from the blood stream. Intramuscular administration has a much slower distribution rate compared to the intravenous, often up to fifteen minutes.
The last method through which buprenorphine can be administered is sublingually. Sublingual administration is not preferred by some practitioners as it cumbersome to administer especially when the patient is in an advanced state of withdrawal (Hales, 2008). Sublingual administration is only possible in stable patients or for home kits where the ability of the patient to administer intravenous or intramuscular doses is questionable. Sublingual administration has many other disadvantages as well, such as the slow rate of absorption usually between 200 and 250 minutes.
Buprenorphine binds tightly to the plasma proteins which increases bioavailability which takes between 25 and 60 hours to be processed by the liver and fully eliminated from the body. The ‘Cytochrome P4503A’ enzyme breaks down the drug in the liver and forms norbuprenorphine as a byproduct (Bolourian, 2010). Buprenorphine is relatively a new drug and has not yet been extensively tested. Its effects on pregnant women are not known and for safety purposes is not recommended for this population. It is not recommended for individuals who are not addicted to opiates because it is a mild opiate and patients who use it may exhibit the addictive properties of conventional opiates.
Methadone
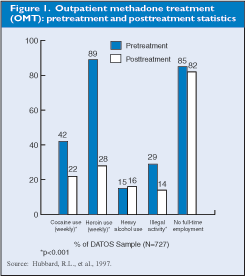
This was the earliest drug that was used in the treatment of opiate addiction. Methadone has been in use for over 30 years, and extensive testing and research has been done on the drug. Methadone treatment is an effective way of treating opiate addiction and the withdrawal accompanying symptoms. The mode of action of methadone is only effective for opiate drugs and cannot be used for any other type of drug addiction. The half-life of methadone is much lower than that of buprenorphine and thus buprenorphine is preferred over methadone. The Food and Drug Administration (FDA) has implemented legislation that promotes the responsible use of methadone to treat opiate addiction.
Methadone has been found to be clinically safe and causes no physiological damage. Studies on the lungs, kidneys, heart, liver and genitals of prolonged users show no signs of damage or deformities which support that the use of methadone is an effective alternative to buprenorphine (Hales, 2008).
Both methadone and buprenorphine occupy brain receptors in the brains of addicts. This causes addicts to become addicted to these drugs instead of to the opiate. Addiction to methadone and buprenorphine are less harmful to the addict because they do not possess similar effects as opiates. Cases of patients who have become addicted to the detoxification drugs are very common; however this type of addiction is preferred as these patients are usually able to carry on with their normal lives (Cowan, 2008). Addiction to buprenorphine and methadone does not cause highs and dizziness as do opiates.
Inpatient detoxification centers
Inpatient detoxification centers are becoming the preferred option for treatment of opioid addiction because these centers offer controlled environments that facilitate fast treatment of opiate addicts. Safe and secure environments protect patients from external factors, and control physical and psychological treatments. Inpatient treatment of opiate addicts is more expensive when compared to outpatient treatment but has been found to yield better results and higher success rates. Studies showed that 74% of all outpatient opioid addiction treatment programs are unsuccessful, whereas 58% of all inpatient opioid are unsuccessful (Magnelli et al, 2010).
This evidence supported that inpatient treatment have a higher chance of facilitating rehabilitation of opioid addicts and justifies the higher costs incurred in this type of treatment. Inpatient treatment also eliminates the abuse of opiates in patients who are under constant care and supervision. Outpatient treatment risks include Subuxone (buprenorphine) dependence related to the decreased self control of opioid addicts who are not well supervised (Renner, 2009).
Program Evaluation of Opiate Addicts
There are various factors that are used to determine the effectiveness of an opiate detoxification program, such as the ability of the drug to treat withdrawal symptoms, the cost effectiveness of the drug, the half-life of the drug, the effect of the detoxification drug on patients of varying ages and genders, the side effects of the drug and the overall safety of the drug.
The current study examined the effects of buprenorphine on opiate addicted patients undergoing detoxification. The study examined the experiences of 200 patients from the center. Demographic information such age, employment status, type of opiate abused, number of years of drug abuse and physical characteristics of the patient were collected.
Hypothesis of the study
The objective of the study was to examine the effectiveness of the detoxification program and determine its effect on opiate addicts, particularly buprenorphine which is extensively used in the center and has replaced methadone as the detoxification drug of choice.
The hypotheses for the study are:
- Ho: There is a correlation between the patient effects observed and the detoxification procedures used at the detoxification centre.
- HA : There is no correlation between the patient effects observed and the opiate detoxification procedures used at the detoxification centre.
Research methodology
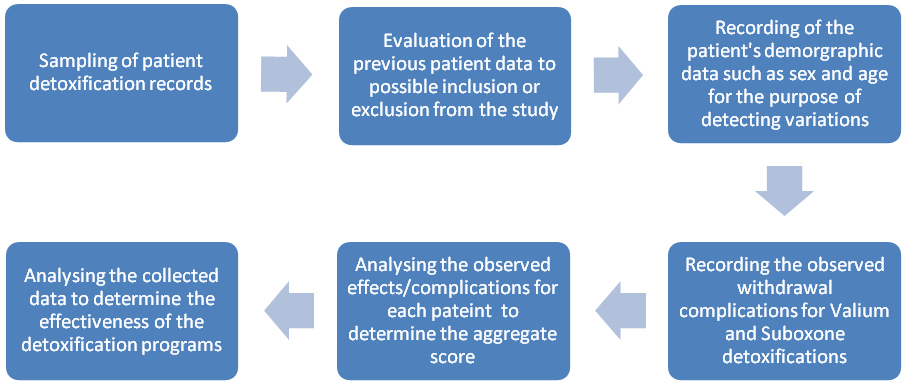
The research was carried out according to a structured plan. This involved the collection of data from patients’ records, evaluation of the data, making records of the collected data and interpretation of the results. Data from a random sample of 200 charts were collected from the center using a table of random numbers. The collected data were recorded into excel sheets. All the necessary details and information that was availed to the researcher was tallied in these sheets. The data was then interpreted and analyzed using SPSS (Statistical Packages for Social Sciences) software
Assumptions of the study
- There is no marked difference in opiate resistance related to the age and gender of patients
- The effects of buprenorphine are similar in each patient
- There is no difference in patient outcomes related to years of abuse.
Findings
Age of opiate addicts
The majority of all opiate addicts, some 64% were found to be below the ages of 40. A few of the patients whose data was collected were above 60 years of age but this was restricted to only 7%. The findings indicated that opiates are a common problem among the young and young adult. The mean age of opiate addicts in the study was 23.4 years. The study showed that people often resort to rehabilitation as a treatment option after the addiction has advanced into serious levels. The ages range from 20 to 30 had the highest number of patients signifying that this age group is most susceptible to opiate addiction.
However this does not mean opiate abuse commences within this age group but is a reflector of a period when the abuser becomes unable to control the habit. The ages 18 to 20 are the introductory years when most patients commence abuse of opiates. The ages 20 to 30 are the maturity phase when abusers graduate into serious addicts.
Percentiles for age
The results indicated that half of all opiate addicts (100) are between 18 years of age and 32 years of age. This is the critical age where most people using opiates seek medical attention. The results showed that 76% of all subjects were between 18 years and 46 years of age. A small percentage (46 patients) was between 46 and 65 years of age.
Status of patients
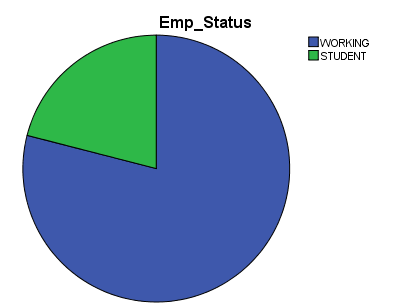
Data collected from the Detoxification Center indicated that most opiate addicts were working citizens with a small percentage being students. This results showed that out of the 200 patients whose information was collected, 79% were working individuals and percentage 16% were students.
A major factor implicated in opiate abuse is stress and pressure either from the work place or the society. Working people face more pressure and are more likely to report more stress as compared to non working people. Family pressure and domestic squabbles are factors that also lead working people into opiate abuse. The patients often look for a way to escape from reality and the unpleasant things that exist in the real world. Opiates offer a temporary escape from personal problems and offer a false feeling of peace and happiness. Importantly working people are able to afford opiates and private detoxification treatment, and this may explain why the majority of opiate addicts in the study were from the working class.
Pulse rates
Qualities of a good detoxification drug is that it should have none or minimal adverse effects on pulse rates of the patient as this can result in fatalities (Junig, 2009). In the subjects of the current study pulse rates were measured before the introduction of buprenorphine, 30 minutes after the induction, two hours after the induction and four hours after the induction. The data were tallied and graphs were prepared using the data.
Sweating and chills
Buprenorphine is reported to cause a marked decrease in sweating among patients during detoxification (Kleber, 2008). Similar findings were found in the current study where patients experienced severe sweating. At 30 minutes after administration of the first dose of buprenorphine, 88% of patients who were suffering from severe sweating had a marked decrease in sweating. At four hours, an additional decrease in sweating occurred. There was a significant drop in the number of patients suffering from severe sweating as time progressed to 4 hours. The number of patients who reported to be free from chills and sweating increased immediately after the administration of the drug. This indicated that the drug was able to rapidly ease symptoms of withdrawal such as sweating.
Buprenorphine has been found to cause a marked decrease in sweating among patients during detoxification (Kleber, 2008). Similar findings were found in the current study where patients experienced severe sweating. At 30 minutes after administration of the first dose of buprenorphine 88% of patients who were suffering from severe sweating had a marked decrease in sweating. At four hours, an additional decrease in sweating occurred. There was a significant drop in the number of patients suffering from severe sweating as time progressed to 4 hours. The number of patients who reported to be free from chills and sweating increased immediately after the administration of the drug. This shows that the drug is able to rapidly ease symptoms of withdrawal such as sweating.
Restlessness
Withdrawal from opiates may cause stiffening and random contraction of the body muscles making the patient unable to sit still or relax. Buprenorphine has been found to relax patients and stop the random contraction of body muscles by promoting smooth muscle relaxation (Silk, 2009). In the current study, before the administration of buprenorphine the majority of patients-(72%) were unable to sit still even for a few seconds and were frequently shifting positions or experiencing extraneous limb movement. Within 30 minutes after fter the administration of buprenorphine, symptoms started to ease and 58% of the patients were able to sit still.
Buprenorphine is at its optimum 2 hours after the first dosage is induced. At this period the patient is most relaxed and at ease. This study showed that buprenorphine starts its action immediately after it has been induced and continues to improve restlessness up to two hours. At four hours, the relaxing and easing effects of the drug have stabilized.
Buprenorphine is, therefore, very useful in relieving restlessness such as shifting and muscle contractions which are a major cause of distress among patients with withdrawal syndrome. This justifies the use of buprenorphine during opiate addiction detoxification as a way of aiding muscle relaxation and improving patient comfort and outcomes.
Pupil size
Buprenorphine is found to ease pupil dilation. Pupil dilation is another common symptom of opiate withdrawal and has the potential to damage the eyes (Cowan, 2008). The ability of buprenorphine to ease pupil dilation also shows its ability of treating other symptoms of withdrawal. Data was collected on the size of pupils of patients and was recorded at 30 minute, 2 hour and 4 hour intervals.
The results showed that buprenorphine reduced the number of patients with severe pupil dilation so that only the rim of the iris was visible and increased the number of patients with normal pupil size. At 2 hours, 64% of the patients had normal pupils and 22% had near normal pupils. At this time only 8% of all the subjects had dilated pupils. Four hours after the first dose was induced the effects of buprenorphine were still evident. This shows that buprenorphine is an effective method of treating pupil dilation and its effects are as strong at four hours as they are in 30 minutes after the first dose is administered.
Bone / joint aches
Patients undergoing opiate detoxification often complain of severe joint pain (Renner, 2009). Patients in the current study reported mild to severe and diffuse joint pain before induction of buprenorphine. After the induction, there was a marked increase in the number of patients complaining of severe to mild joint pains. 30 minutes after the first induction, 51% complained of mild pains while 38% did not feel any pain. At 2 hours after induction, most of the patients (63%) were free from joint pain. At four hours, the majority of these patients had been relieved of the joint pain.
This study showed that buprenorphine eases the occurrence of joint pain among patients and reduces the severity of pain in patients who are already suffering from joint pain. This is a desirable quality of buprenorpine and this should be listed as one of its positive effects. Based on the findings of this study appropriate pain relief measures to relieve joint pain should be considered when administering buprenorphine for opiate detoxification.
Running nose and tear development
Patients undergoing opiate detoxification typically report a great deal of nasal stiffness and rhinorrhea (Langrod, 2008).The induction of buprenorphine resulted in an increase of patients who claimed not to have running noses and who had some slight nasal stuffiness. There was also a decrease in the number of patients who had mild running noses and those who had constant running of noses.
These changes were seen 30 minutes after the first induction and were more pronounced 2 hours after the first dosage. Similar to other withdrawal symptoms, the effectiveness of buprenorphine in suppressing tearing and production of nasal mucous stabilized with time. Four hours after the first dose of buprenorphine was administered fewer patients complained of stuffy noses as compared to before the drug was administered. There was a huge reduction in the number of patients who had constant running noses and noses that were running; from 79% to 6% as compared to before the drug was administered.
Effects of buprenorphine of the gastrointestinal tract
Gasrointestinal (GI) discomfort ranging from mild cramping to severe cramping, diarrhea and vomiting are reported by patients undergoing opiate detoxification (Kleber, 2008). In the current study, buprenorphine had an overall effect on the state of the patient’s gastro intestinal tracts. Within 30 minutes after the initial dosage of the drug there was a reduction in the number of patients complaining of vomiting and multiple diarrhea episodes from 140 to 25. At two hours the efficacy of the drug remained stable and there was a slight decrease in nausea and multiple diarrhea cases.
The effects of the drug stabilized at four hours and were similar to those recorded at two hours. These findings support the claims that buprenorphine is an effective drug to reduce GI symptoms associated with opiate detoxification. The positive effects of the drug on GI symptoms do not fade with time as with other symptoms. The effects of buprenorphine on nausea and vomiting impulses at four hours were almost as pronounced as at 30 minutes after the first induction.
Anxiety and irritability
Buprenorphine has been found to have instant relief for patients suffering from irritability and restlessness during opiate detoxification. Thirty minutes after the induction of the drug, there was a decrease in the number of patients who were obviously irritable and severely irritable from 165 to 51 patients. Data were collected at three intervals and there were significant variations in the irritability levels of the collected samples. The results showed that four hours after the first dose was administered, there was a substantial decrease in irritability levels of the patients with 58% of the patients not being irritable and 30% slightly irritable.
Only 12% (26 patients) were still obviously irritable or extremely irritable four hours after the first dose. Therefore buprenorphine can be said to be a treatment option for patients suffering from extreme irritability. Opiate addicts are usually very anxious and irritable and sometimes therapy is not possible in such situations, therefore the ability of buprenorphine to reduce irritability and anxiety among the patients makes it a suitable and very useful drug for use in detoxification programs.
Yawning
After the administration of the first dose of buprenorphine there was considerable change in the yawning characteristics of the patients. Data collected at 30 minutes after the first dose shows some change in yawning behavior of the patients. Four hours after the first dose had been induced the number of patients who were yawning, yawned once or twice during the interview, yawned three or more times and those who yawned multiple times had undergone great change.
There was an increase in the number of patients did not yawn during the interview from 27% to 57%. This results indicated that buprenorphine had considerable effects on reducing yawning among patients. Yawning does not have any harmful effects to the patients but it is a useful tool to study of the effects of buprenorphine on opiate addicts, as it is a common and annoying withdrawal symptom of opiate addiction which is easily observed by the clinician.
Total score
Summary Statistics for v59_a
Buprenorphine had a total score of above average. On a scale of one to eight the drug scored a mean of 5.64. This is satisfactory performance indicated that the be useful in the treatment of opiate addiction.
Data analysis
Chi square analysis was used to determine the effectiveness of the chosen hypothesis. This analysis was carried out on the readings of a few symptoms so as to test the hypothesis. The formula used was:
Chi= (o-e)2/e
Where o = observed results
e = expected results
In this study, there was a 5% chance that the observed readings were incorrect. However, even if there was a variation of 5% in the data due to errors the alternative hypothesis would still hold true. It is for this reason that the hypothesis: There is a correlation between the patient effects observed and the detoxification procedures used at the Detoxification Centre, was accepted.
Conclusion
Buprenorphine has been found to be an effective method of treating patients who have become addicted to opiates. Data were collected by reviewing 200 charts from the center and the data were analyzed to evaluate the effect buprenorphine had on opiate addiction withdrawal symptoms. Buprenorphine was been found to have notable effects on opiate addiction withdrawal symptoms. The use of buprenorhine in the detoxification procedure resulted in a significant changes in the symptoms of the patients. This study supports the use of buprenorphine in the rapid withdrawal of patients who have opiod addiction. Effects noted in the study include that use of buprenorphine:
- Resulted in an decrease in pulse rates
- Reduced sweating in the patients
- Eased pupil dilation
- Prevented the formation of joint pain in normal patients and eased the pains in those who are already suffering from pain
- Normalized running nose and tear production
- Eased nausea and vomiting
- Reduced anxiety, restlessness and enables patients to relax
- Eased tremors
- Prevented unnecessary yawning
Buprenorphine has a half-life of between 25 hours and 72 hours. The drug is able to ease severe symptoms that are often accompanied with opiate withdrawal. The data collected from the study shows that buprenorphine is effective against most withdrawal symptoms and can be effectively be used to treat these symptoms for prolonged periods of time.
The main buprenorphine drug used in the center was Suboxone. This is a reliable drug that has been found to be helpful to patients. Buprenorphine is also administered in small but effective doses of 8mg per patient. These doses have been found to be effective and only in isolated cases were 16mg doses are used. A small percentage (2%), of all the patients in the center required 16mg doses which indicated that small doses of buprenorphine are effective in treating withdrawal symptoms. After a period of using buprenorphine ‘Subuxone’ the patient may decide to taper off the drug. This should be a careful process that has to be decided by the patient and healthcare provider.
The taper process should be done carefully so as to avoid relapse. The taper period should be accompanied by proper counseling of the patient so as to provide the motivation and drive needed to quit the habit. A slow taper is recommended as it allows the patient’s body to slowly adjust to the falling levels of opioids. The patient and healthcare provide should address the issues of relapse quickly by monitoring sumptoms and offering small doses of buprenorphine. Subuxone is the main type of detoxification drug used in the center in this study and has been supported as a treatment for opioid addiction.
The study also shows that treatment of opioid addiction is possible in controlled environments, the center is an example of where the safety of the patients is assured and an environment that facilitates treatment is provided. The patients are kept in a luxurious environment where medication and psychological health counseling is provided. The center has a team of nurses and medical personnel who are assigned to assist the patients
Inpatient detoxification has been found to be most effective and thus a model similar to the Detoxification Center is recommended for opioid addiction treatment. The study shows that inpatient facilities allow for proper treatment and personalized care of each patient. Outpatient treatment services are often marred by interrupted /uncontinuous administration of drugs to the patients.
The public policy in America for treatment of opioid addiction needs to be addressed. There has been minimal success of outpatient treatment services documented in the literature. Instead more facilities should be developed using the model described by the inpatient center for treatment of opioid addiction.
References
Bolourian, S. (2010). Buprenorphine: A Guide for Readers. New Jersey, NJ: Dane Publishing.
Courtwright, D. (2009). Dark paradise: a history of opiate addiction in America. New York, NY: Harvard University Press.
Cowan, A. (2008). Buprenorphine: combatting drug abuse with a unique opioid. Michigan, MI: Wiley-Liss.
Doweiko, H. (2006). Concepts of Chemical Dependency. California, CA: Cengage Learning.
Hales, R. (2008). Study Guide to Substance Abuse Treatment. Arlington, VA: American Psychiatric Publishing.
Junig, J. (2009). User’s Guide to Suboxone: Taking buprenorphine for opiate Dependence. Wisconsin, WI: Terminally Unique Publishing.
Kleber, H. (2008). The American Psychiatric Publishing textbook of substance abuse treatment. Arlington, VA: American Psychiatric Publishing.
Langrod, J. (2008). The Substance Abuse Handbook. Philadelphia, PA: Lippincott Williams and Wilkins.
Magnelli, J., Biondi, B., and Calabria, K., (2010). Safety and efficacy of buprenorphine/naloxone in opioid dependent patients. California, CA: Clinical Drug Investigations.
Maremmani, I. (2010). Buprenorphine-based regimens and methadone for the Medical treatment of opiate addiction. New York, NY: Med Publishers.
Marquete, P. (2008). Buprenorphine Therapy of Opiate Addiction. New Jersey, NJ: Humana Press.
Millman, R. (2007). Substance abuse: a comprehensive textbook. Philadelphia, PA: Lippincott Williams and Wilkins.
Orman, J., and Keating, G. (2009). Buprenorphine/Naloxone: a review of its use in treatment of opiate addiction. New Jersey, NJ: Humana Press.
Renner, J. (2009). Handbook of Office-Based Buprenorphine Treatment of Opioid Dependence. Arlington, VA: American Psychiatric Publishing.
Silk, K. (2009). Cambridge Textbook of Effective Treatments in Psychiatry. New York, NY: Cambridge University Press.
Strain, E. (2005). The treatment of opioid dependence. Maryland, MD: John Hopkins University Press.
Thakkar, V. (2008). Addiction. New York, NY: Infobase Publishers.
World Health Organization. (2009). Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence. Geneva: World Health Organization.