Introduction
Tuberculosis (TB) is an acute or chronic infectious disease that has claimed many lives for centuries. It has been changing for years, making it difficult to have a single method of curing the disease. In recent years, tuberculosis has been associated with multiple deaths worldwide, with developing countries facing a significant problem in handling the disease. The United States has several infections, and the center for control and prevention (CDC) has been identifying various ways of handling the infection. This essay focuses on tuberculosis infection, prevention and control, surveillance, epidemiology, and significant events.
Tuberculosis (TB) Infection
It is a contagious disease caused by Mycobacterium tuberculosis that affects the lungs and can spread to other body organs such as the spine and brain. There are two main types of TB: latent TB and active TB. Latent TB is a type of tuberculosis that is not contagious despite an individual having the bacteria in the body (Furin et al., 2019). Latent TB usually waits for an individual to develop weak immunity to get active. Active TB is a type of tuberculosis that is active and makes one sick. However, the active TB signs and symptoms include weight loss, chills, coughing blood, loss of appetite, chest pains, fever, and feeling exhausted most of the time.
The CDC statistics show that in 2017, there were more than 10 million TB cases, with a rate of 133 per 100,000 people (MacNeil et al., 2017, p. 263). This was a decline when compared to the previous year’s cases. The decline was estimated to be 3.9% in 2016 to 1.57% in 2017, with a case fatality of 15.7% with a 0.5% decline (MacNeil et al., 2017, p. 263). The infection was significant among individuals with HIV, accounting for 920,000 cases, representing 9% of the total cases (MacNeil et al., 2017, p. 263). The overall death of people with TB among HIV patients was 300,000, with a case fatality of 32.6% (MacNeil et al., 2017, p. 263). Rifampicin-resistant TB (RR-TB) cases and multi-drug resistant TB (MDR-TB) cases accounted for 558,000 incidents (MacNeil et al., 2017, p. 263). The total death from this group was 230,000 representing a case fatality of 41% (MacNeil et al., 2017, p. 263). The above statistics are shown in table 1.0 in the appendix.
Tuberculosis is an airborne infection that implies that the disease is transmitted through airborne particles. When an infected individual sings, coughs, shouts, or sneezes, the generated nucleic gets suspended in the air particles for various hours. When these particles get in contact with a person through inhalation or swallowing, they are transferred to the alveoli of the lungs. When in the lungs, the incubation period for the tuberculosis bacteria is about twelve weeks (Behr et al., 2018). An infected individual becomes contagious during this period so long as the bacteria are in the sputum. Individuals are usually contagious for about two to three weeks after the incubation period.
Tuberculosis treatment involves patients taking a combination of medications based on patient circumstances considering if they have had the disease before or not, which goes up to 6 months with no interruption. These patients have to take a minimum of three drugs as part of the first treatment. This is because fewer drugs can lead to drug-resistant Tb development (Al-Saeedi & Al-Hajoj, 2017). If the patient has never received treatment before, the doctor will have to prescribe Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol (Mase & Chorba, 2019). This follows the probability that the bacteria will be sensitive to all medication and it will not respond to the patient’s body.
Patients receive isoniazid medication with each tablet containg100mg of isoniazid, and adults take up to 300mg per day. The drug has no severe effects and only causes worsening acne, irritability, lack of concentration, and tiredness (Al-Saeedi & Al-Hajoj, 2017). However, the medication can affect the patients’ liver, and they will have to consult their doctor if they begin to experience nausea, yellow eyes or skin, vomiting, dark-colored urine, and stomach pain. Moreover, patients will start to feel a tingling in their toes and fingers and will have to take Vitamin B6 to curb it. Additionally, drug interactions can take place with the epilepsy anti-convulsant medication.
Rifampicin drug has 150mg and 300mg strength capsules with varying colors indicating strengths and brands. These capsules have to be taken one hour before or two hours after the patients eat (Gill et al., 2022). The medication causes an orange-reddish coloration of saliva, sweat, semen, and urine. Its primary side effects include lack of appetite, stomach discomforts, nausea, and at times diarrhea and vomiting. Rifampicin interacts with other drugs, including morphine, warfarin, digoxin, methadone, and oral diabetic medication.
Pyrazinamide medication has 500mg large white tablets enriched with Pyrazinamide. The dosage of this drug is prescribed depending on the patient’s weight (Gill et al., 2022). Its main side effects are flushing lack of appetite, nausea, skin itchiness and rashes, and pain in joints. Moreover, patients are advised to contact their physician if they encounter stomach pain, yellow eyes or skin, and vomiting. Lastly, ethambutol contains 400mg and 100mg tablets prescribed, considering the patient’s weight (Gill et al., 2022). The patients are advised to inform their doctors if they observe a change in eyesight or blurred and changes in color vision.
Two main methods are used to test for tuberculosis, including skin and blood tests. The skin test method involves the injection of the tuberculin at the lower arm’s skin. After 48 to 72 hours, the inactive TB protein on the skin is checked for identification depending on the swelling. A negative diagnosis’s cut-off value is 5mm and 15mm or more for a positive diagnosis. Those who get an induration of at least 5mm may be positive for Tb if they have HIV and have been previously treated for Tb, received an organ transplant, or have been taking antidepressants (Zaheen & Bloom, 2020). Moreover, an induration of at least 10 mm may indicate a positive TB diagnosis if the patient lives in a risky environment, uses injected drugs, is below four years old, and works in a medical facility.
The blood test is done by interferon-gamma release assays (IGRAs). A positive TB blood test implies that an individual is infected, while a negative blood test implies that an individual is not infected. The Quantiferon-TB Gold Plus (QFT-Plus) has a cut-off value of 0.35 IU/mL that is used to interpret the diagnosis of tuberculosis as being negative or positive (Uzorka et al., 2018). The (QFT-Plus) is used to diagnose tuberculosis and is an interferon-gamma assay used in the blood test. Moreover, patients will have to get chest X-rays when they get a positive diagnosis of TB or test positive every 5 to 10 years and help show advanced pulmonary tuberculosis (Abbas, 2018). Multiple negative results are significant as they provide more information to make medical decisions, prevent irrelevant TB treatment, and advance testing for another diagnosis (Zaheen & Bloom, 2020). This is because one negative result cannot be used in providing a conclusive result to rule out tuberculosis, specifically if there was high or moderate clinical suspicion of the disease.
Prevention and Control
There are various methods that public health professionals employ to curb and prevent tuberculosis cases. First, healthcare facilities are given access to radiology tests and laboratories. Second, infected individuals receive treatments to prevent the spread of the disease. Third, medical staff is trained, enabling them to manage the cases with minimal risk (Cole et al., 2020). The population-level disease control measure is usually implemented to prevent the further spread of the infection. At this level, the infected individuals are identified, and those with active tuberculosis are treated, making the infection non-contagious. The individuals who have had contact with the TB patients are screened to ensure that they do not have active TB (Li et al., 2017). Individuals that are identified to be at risk are then subjected to treatments. Various awareness procedures are set up to enable the public members to avoid certain activities that may lead to the spread of TB.
In the fight against TB, Bacille Calmette-Guérin (BCG) vaccine has been developed. The vaccine contains attenuated TB bacteria that boost the immune system. This vaccine is mainly given to children and infants in regions prone to TB (Madan et al., 2020). However, the vaccine does not usually prevent individuals from getting infected. Furthermore, the vaccine is only administered to children that have tested negative and are frequently exposed to TB. Also, the children who cannot be separated from the infected adults or are not properly treated are among the considered group for vaccine administration. Other included groups are healthcare workers working in areas with a high proportion of TB patients with strains resistant to rifampin and isoniazid.
The vaccine’s efficacy is approximately 70% to 80% and is suitable for severe types of TB such as meningitis tuberculosis. Conversely, it is less effective in tuberculosis, which affects the lung. Additionally, the vaccine cannot be used in individuals with low immunity because it replicates quickly, leading to severe infection (Renardy & Kirschner, 2019). This group includes breastfeeding mothers that have a suppressed immunity when pregnant. The current TB vaccine (BCG) can only be used as a pre-exposure. It is only given to individuals who have not been infected previously with tuberculosis to prevent upcoming infections.
Quarantine and isolation are significant measures in preventing the further spread of contagious infections. Quarantine is not applied in controlling TB because individuals with latent TB do not pose any risk of transmission. However, isolation is a critical measure in managing the spread of TB. TB patients pose a significant threat as the bacteria are airborne (Xin et al., 2021). The individuals are usually isolated while receiving treatment, and Isolation is stopped within a few weeks of receiving treatments. The post-exposure prophylaxis for individuals developing active TB can be a supplement in controlling the TB. Currently, chemoprophylaxis is the most used method in TB Post-exposure prophylaxis. This preventive treatment has significant efficacy in managing the disease.
Surveillance
Case definitions tend to vary from one health organization to another. World health organization provides various case definitions and classifications. The first case is a bacteriologically confirmed TB case determined by the outcome of the biological specimen. The identified cases are reported regardless of whether the treatment has been administered or not. The second case is the clinically diagnosed TB, where the patient has been diagnosed with active TB or the medical practitioner has decided the patient undergoes complete TB treatment (WHO, 2020). This includes X-ray diagnosis areas that reveal abnormalities and extra pulmonary cases that the laboratory has not yet confirmed. Furthermore, subsequent cases of positive bacteriology before or after treatment are also classified as bacteriologically confirmed. The clinically diagnosed TB cases are classified into HIV status, previous treatment history, anatomical site of disease, and drug resistance. Tuberculosis is nationally notifiable in the US, and it is reportable in the state of Nevada.
Epidemiology
Individuals vary significantly in the way TB affects them. Those who develop TB symptoms after being infected by the Mycobacterium even before the immune system fights the infection and those that take a long time before they get sick because of a robust immune system. Approximately 5% to 10% of individuals infected with TB end up developing the infection at some point in life. Individuals at a higher risk of getting TB are categorized into those infected by TB recently and those that have developed a condition that reduces the strengths of their immune system (Silva et al., 2018). Those infected by TB recently include individuals who have been in contact with a person having active TB, people who have migrated from areas with higher cases of TB, and children who have tested positive and are below five years of age. Additionally, some groups have high rates of tuberculosis, such as individuals with HIV infections and homeless people (Shimeles et al., 2019). The group with the compromised immune system includes individuals infected with HIV, drug users, people undergoing medical treatments such as organ transplants, diabetes mellitus patients, individuals suffering from head and neck cancer, and people with low body weight.
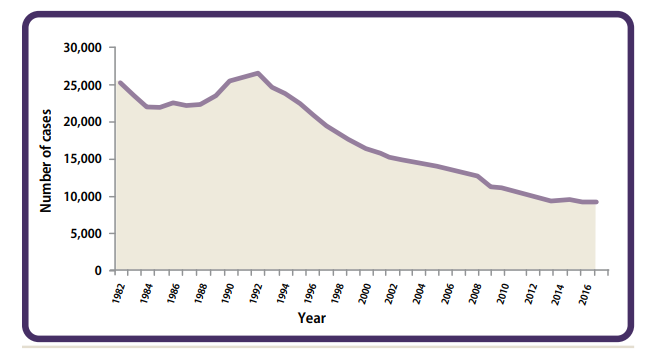
Reporting of TB in the United States began in 1953 because of the increased cases of TB. During this period, the US had more than 84,000 cases of tuberculosis (CDC, 2019). From 1953 to 1984, the number of TB infections decreased significantly, with an average rate of 6% every year (CDC, 2019). In 1985, the total cases of TB were at their lowest with 22,201 cases (CDC, 2019). TB cases began to rise in 1986 after a significant period since 1953. From 1985 to 1992, the number of TB cases increased from 22,201 to 26,673, representing an increase of approximately 20% (CDC, 2019). However, in 1993, the number of infections decreased, which was experienced for 21 years until 2014 (CDC, 2019). A slight increase in the number of cases was noted in 2015. In 2017, the United States reported a significantly low number of TB cases since it began reporting in 1953. The above statistics are shown in figure 1.0 in the appendix.
Despite the downward trend and reduced number of TB cases in the US, TB has become a critical issue in the US states as in some areas, the number of cases is increasing significantly. Most of the cases are associated with untreated latent TB infection. The Asians and the African America are the most affected group in the US as they have a high number of TB cases compared to the White (CDC, 2019). CDC (2019) shows that 27% of the reported TB cases were among the Hispanics, 21% of the cases among the African Americans, despite the group constituting only 12% of the American population. 36% were among the Asians, who constitute 6% of the population and 1% among the American Indians, who represent 1% of the population, and less than 1% among the Pacific Islanders, who constitute less than 1% of the American population (CDC, 2019).
From a global perspective, tuberculosis is a significant problem that affects a large population. In 2020, approximately 1.5 million people died from the infection, including 214,000 people already infected with HIV (“Tuberculosis (TB),” 2022). TB is identified as the 13th leading cause of death, and on the infectious level, it is second after COVID-19. The WHO 2020 report shows that on a gender basis, men are highly infected by TB compared to women and children. Men constitute 5.6 million, women 3.3 million, and children 1.1 million (“Tuberculosis (TB),” 2022). The distribution of TB does not vary with age, as TB can infect anyone at any age.
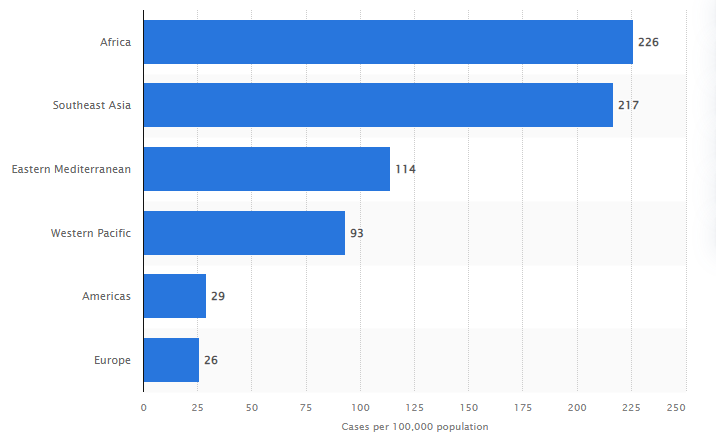
From figure 2.0 in the appendix, Africa had 226 new cases of tuberculosis which was the highest number compared to other regions (Statista, 2021). It was followed by Southeast Asia, which reported 217 new cases of the disease. The third region. Eastern Mediterranean had only 114 new instances of Tb in the same year (Statista, 2021). Western Pacific, which is the fourth region, reported 93 cases. Finally, America had 29 cases, and Europe reported 26 cases, ranking the lowest of the six regions (Statista, 2021).
The burden of this disease is enormous as more than 30 countries account for 86% of the new cases (“Tuberculosis (TB),” 2022). The top countries include India, China, Nigeria, Philippines, South Africa, Indonesia, Bangladesh, and Pakistan. TB has no specific geographical position as it is present in all parts of the world. The WHO 2020 report shows that South East Asia constitutes 43% of new cases, the African region 25%, and the Western Pacific area 18% (“Tuberculosis (TB),” 2022). Various studies have shown that TB is a seasonal infection and is high during the spring period and lowest during late fall. This trend is also proven in the United States by various researchers.
Special Topics and Significant Events
The major tuberculosis outbreak happened between 1800 and 1990 in North America and Europe. 70%-90% of North American and Europe urban populations contracted the disease by the late 19th century (Barberis et al., 2022). In the United States alone, there were 84,304 cases in 1953 and 79,775 in 1954. In Western Europe, TB was a significant problem during the 18th century as it had a mortality rate of 900 deaths per 100,000 people. It mainly affected the youth and was titled “the robber of the youth.” During the Industrial Revolution, there were significant problems such as poorly ventilated housing, malnutrition, primitive sanitation, and overcrowded housing (Barberis et al., 2022). These factors were linked with the development of tuberculosis. The period 1838 to 1839 had a significant number of death of employees and merchants who died of TB (Barberis et al., 2022). In the early 20th century, TB claimed a significant number of lives in North America and most of the urban population of Europe. More than 80% of the infected individuals developed active TB, which made them succumb to death.
There has been a significant development in the fight against TB. Various diagnostic technologies have been developed, as reported by the WHO. Detection of TB that is resistant to the antibiotics such as rifampicin and isoniazid has been enhanced by the development of automated Nucleic Acid Amplification Tests (NAATs) (“WHO,” 2021). Furthermore, the technology promotes detecting TB resistance in other cases, such as second-line anti-TB agents and pyrazinamide. Moreover, there have been recent developments regarding TB with a common antibiotic known as doxycycline, which was found beneficial in increasing the disease’s recovery rate. It was discovered that the use of the antibiotic together with Tb medication treatment resulted in the reduction of lung cavities size and accelerated lung recovery markers (Miow et al., 2021). Additionally, a trend was observed in 2020 and 2021with, with a drop in tuberculosis cases following the COVID-19 pandemic worldwide. For instance, the United States reported a decline in TB diagnoses by 20% in 2020 and 13% in 2021 compared to the previous years before the pandemic (CDC, 2022). This resulted from COVID-19 regulations, including the constant wearing of masks and maintaining six feet social distance.
Conclusion
In conclusion, the essay has portrayed various factors surrounding tuberculosis (TB). It is a contagious disease that affects a significant portion of the USA population and the global community. Currently, the infection hugely affects Asian and African countries. Despite its reduction in infection rates, there are areas where individuals are hugely affected by this condition. Identification of patients infected by TB is an essential measure in curbing its spread. Isolation is an important step in the fight against TB since the disease is airborne and highly contagious. The history of TB shows that it is necessary for the condition to be given maximum attention as it leads to multiple deaths when not treated. It is not selective as it affects individuals of all age groups. However, various antibiotics have been developed which help treat the infection.
References
Abbas, U. (2018). The Radiological Diagnosis of Pulmonary Tuberculosis (TB) in Primary Care. Journal of Family Medicine and Disease Prevention, 4(1), 1-7. Web.
Al-Saeedi, M., & Al-Hajoj, S. (2017). Diversity and evolution of drug resistance mechanisms in Mycobacterium tuberculosis. Infection and Drug Resistance, Volume 10, 333-342. Web.
Barberis, L., Braggazi, N., Galluzo, L., & Martini, M. (2022). The history of tuberculosis: From the first historical records to the isolation of Koch’s bacillus. Journal of Preventive Medicine and Hygiene, 58(9), 9-12. Web.
Behr, M., Edelstein, P., & Ramakrishnan, L. (2018). Revisiting the timetable of tuberculosis. BMJ, 1-8. Web.
CDC. (2022). Effect of COVID-19 on Tuberculosis in the U.S. Centres for Disease Control and Prevention. Web.
Centers for Disease Control and Prevention (CDC). (2019). Epidemiology of Tuberculosis (pp. 1-36). Web.
Cole, B., Nilsen, D., Will, L., Etkind, S., Burgos, M., & Chorba, T. (2020). Essential components of a public health tuberculosis prevention, control, and elimination program: Recommendations of the advisory council for the elimination of Tuberculosis and the National Tuberculosis Controllers Association. Center for Disease Control and Prevention (CDC), 69(7), 1-27. Web.
Furin, J., Cox, H., & Pai, M. (2019). Tuberculosis. The Lancet, 393(10181), 1642-1656. Web.
Gill, C., Dolan, L., Piggott, L., & McLaughlin, A. (2022). New developments in tuberculosis diagnosis and treatment. Breathe, 18(1), 1-15. Web.
Li, J., Chung, P., Leung, C., Nishikiori, N., Chan, E., & Yeoh, E. (2017). The strategic framework of tuberculosis control and prevention in the elderly: a scoping review towards End TB targets. Infectious Diseases of Poverty, 6(1), 1-9. Web.
MacNeil, A., Glaziou, P., Sismanidis, C., Maloney, S., & Floyd, K. (2017). Global Epidemiology of Tuberculosis and Progress Toward Achieving Global Targets, 68(11), 263–266. Web.
Madan, M., Pahuja, S., Mohan, A., Pandey, R., Madan, K., Hadda, V., Tiwari, P., Guleria, R. & Mittal, S. (2020). TB infection and BCG vaccination: are we protected from COVID-19? Public Health, 185, 91-92. Web.
Mase, S., & Chorba, T. (2019). Treatment of Drug-Resistant Tuberculosis. Clinics in Chest Medicine, 40(4), 775-795. Web.
Miow, Q., Vallejo, A., Wang, Y., Hong, J., Bai, C., & Teo, F. et al. (2021). Doxycycline host-directed therapy in human pulmonary tuberculosis. Journal of Clinical Investigation, 131(15), 1-15. Web.
Renardy, M., & Kirschner, D. (2019). Evaluating vaccination strategies for tuberculosis in endemic and non-endemic settings. Journal of Theoretical Biology, 469, 1-11. Web.
Shimeles, E., Enquselassie, F., Aseffa, A., Tilahun, M., Mekonen, A., Wondimagegn, G., & Hailu, T. (2019). Risk factors for tuberculosis: A case–control study in Addis Ababa, Ethiopia. PLOS ONE, 14(4), e0214235. Web.
Silva, D. R., Munoz-Torrico, M., Duarte, R., Galvão, T., Bonini, E. H., Arbex, F. F., Arbex, M. A., Augusto, V. M., Rabahi, M. F. & Mello, F. Q. (2018). Risk factors for tuberculosis: diabetes, smoking, alcohol use, and the use of other drugs. Jornal Brasileiro De Pneumologia, 44(2), 145-152. Web.
Statista. (2021). Tuberculosis incidence worldwide by region 2019 | Statista. Statista. Web.
Tuberculosis (TB). Who.int. (2022). Web.
Uzorka, J., Bossink, A., Franken, W., Thijsen, S., Leyten, E., & van Haeften, A. et al. (2018). Borderline QuantiFERON results and the distinction between specific responses and test variability. Tuberculosis, 111, 102-108. Web.
WHO announces updates on new molecular assays for the diagnosis of tuberculosis (TB) and drug resistance. Who.int. (2021). Web.
WHO. (2020). Definitions and reporting framework for tuberculosis (pp. 1-47). Web.
Xin, H., Jin, Q., & Gao, L. (2021). Conditional expanding post-exposure prophylaxis: a potential new tool for tuberculosis control. ERJ Open Research, 7(1), 1-6. Web.
Zaheen, A., & Bloom, B. (2020). Tuberculosis in 2020 — New Approaches to a Continuing Global Health Crisis. New England Journal of Medicine, 382(14), 1-9. Web.
Appendix
Table 1.0: Case fatality