Introduction
Whitaker and Baranski described occupational health nursing as “a frontline role involving a range of aspects, namely: clinician, specialist, manager, coordinator, advisor, health educator, counselor and researcher” (Oakley, 2008, p.1). At the same time, the discipline can be seen to be at the forefront in addressing the question of how effective occupational health nurses can contribute to the improvements in public health by making a difference to the health, safety, and well-being of the working community. In addition, the relationship between work and health has been described as a two-way process in which the working environment can affect the health of the worker and in turn, the worker’s state of health may have an impact on his or her ability to perform the tasks for which he or she is employed.
Occupation health nursing as a discipline, like other recognized disciplines, has utilized theories and models in addressing issues in the field. The theories largely are composed of concepts and propositional statements which connect these concepts in a systematic and elaborative way; moreover, being products of science, they constitute a central part of the knowledge base for professionals in the field. In this paper, emphasis will dwell on the occupational health nursing model and how it can be applied in nursing practice, nursing research, nursing leadership, nursing management, and nursing education.
Metaparadigms in nursing
Johnson defines metaparadigm as a “concept that is extremely general, one that serves to define an entire world of thought” (Johnson, n.d). Jacqueline Fawcett (1984; cited in Johnson, n.d), in her famous work, “Analysis and Evaluation of Conceptual Models of Nursing” developed four main meta paradigms of nursing and which have come to serve in guiding the larger theoretical universe of the nursing profession (Johnson, n.d). The four meta paradigms are; person, health, environment, and nursing.
Person
In nursing, the metaparadigm of a person is the patient who is subjective and unique not objective, predictable, and calculating. The patient at the same time is considered to have distinct human needs which are biophysical, psychophysical, psychosocial, and interpersonal (Johnson, n.d). More so, the patient needs to be valued, respected, nurtured, understood, and assisted. The person at the same time functions as a whole whereby there is no division among the mind, body, and spirit and they are influenced by the external environment.
Environment
The environment is seen as a person’s significant others and the physical surroundings together with other settings in which nursing takes place. The environment is vital to holistic healing that includes; mental, physical, social, emotional, spiritual, developmental, protective, and supportive environments which become conducive to a patient’s health and wellbeing. Furthermore, the environment affects both patients and nurses within a caring-healing interaction. In most cases environment ranges from the patient’s home to the clinical agencies and society as a whole (Johnson, n.d).
Health
Health can be viewed in holistic terms as the unity that connects the physical, social, mental, and spiritual self where all parts work interdependently. Health also is influenced by a patient’s unique life experiences and wholeness; health may include the patient’s physical, social, aesthetic, and moral realms and not only behaviors or physiology (Johnson, n.d).
Nursing
The metaparadigm concept of nursing is seen as the actions that are taken by the nurses on behalf of the patient and at the same time the goals or outcomes of nursing actions. Johnson observes that “it is an intensely ethical and emotional paradigm that goes to the root of nursing as a profession with its own set of rewards” (Johnson, n.d). At the same time, nursing actions can be regarded to involve a thorough process of “assessment, labeling, planning, intervention and evaluation” (Songkham et al., 2006).
Occupational Health Nursing Model
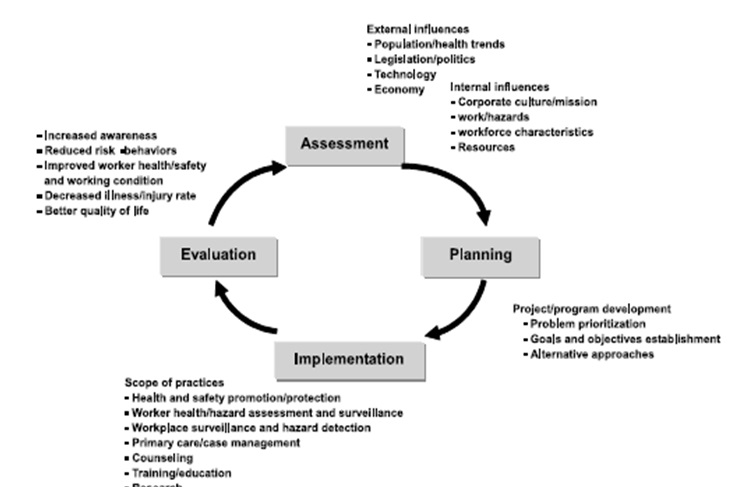
In developing a conceptual framework for occupational health nursing practice, a conceptual framework for occupational health programs and services that have been suggested by Rogers (2003) has been adopted. Rogers’s model identifies the various components of occupational health nursing and states that its goal is to improve, protect, maintain and restore the health of the workforce within a legal and ethical framework. Therefore, it is the context of practice-the-workforce within a legal or ethical framework that separates the goal of occupational health nurses from other nurses. Rogers further suggests that occupational health nurse practice is influenced by conditions in the work setting such as the availability of resources, corporate culture, work hazards, and workforce characteristics. Moreover, these influences operate within a framework of economic, population, and health trends, legislation and politics, and technology. The model is underpinned by a philosophy of occupational health nursing practice and a definition of occupational health nursing.
Assessment
The occupational health nurse has the responsibility to assess the health and safety needs of the worker, the working group, and the work environment. In doing these, the nurse participates in collecting information that is related to the actual and potential health and safety status of the worker, the working group, and the work environment (Songkham et al., 2006, p.3). Additionally, the collection of information may adopt different data gathering techniques such as; observation, interview, health assessment, survey, documentation search, investigation, and consultation. Collected information largely dwells on the state of health and the likely relationship with the work environment, the health history, occupational history, the health and safety hazards that include biological, chemical safety, psychosocial, physical, and ergonomic hazards; existing hazards control measures and emergency potential and preparedness.
Planning
Generally, occupational health nurse develops plans that aim at meeting actual and potential health and safety needs of the worker, the working group, and the work environment. Here, the nurse sets priorities, plans interventions largely depending on assessment and analysis of data as well as plans interventions based on current and relevant research results and any other health and safety information, makes consultations with the client, formulates a nursing plan with goals and objectives that are achievable and lastly, makes contributions to policy and program planning (Songkham et al., 2006, p.4).
Implementation
The occupational health nurse must implement measures that promote, enhance, maintain and restore the health and safety of the worker, the working group, and the work environment. The nurse does these by maintaining open and effective communication with the client, maintaining a comprehensive and current record of interventions, providing continuous health and safety promotion programs that intend to increase the client’s awareness of risks and hence promote positive health and safety practices, conducting surveillance programs that aim to detect, monitoring and intervening in actual and potentially hazardous situations and lastly, participating in the evaluation of environmental data to determine appropriate action (Songkham, et al., 2006, p.4).
Evaluation
Occupational health nurse participates in a systematic evaluation of programs and needs to be conducted periodically to find out its goal achievement. In doing this, the nurse evaluates data incorporated into the assessment phase of the nursing process and makes use of reliable and valid data collection techniques such as the walk-through assessment, worker survey, statistical information, incidence records, performance evaluations, and also the health records (Songkham, et al., 2006, p.4).
Focus and scope
Various considerations have to be put in place in developing a conceptual framework for occupational health nursing practice, for example, consideration of health, the role of nurses, the role of employees, and how the nurse and employee interact to maintain health (Morris, n.d). In many instances, occupational health nursing incorporates a critical philosophy of considerate and appreciation for the individual worker, the profession and function of the occupational health nurse, and the fundamental view of health. The author notes that the cost of health care is rising and as a result, there is a tendency in the shift of nursing care in hospitals towards an emphasis on community nursing care that is largely focusing on preventive health education programs (Morris, n.d). Therefore, the workplace has become one of the best places in the larger community where health screening, education on health, and programs to promote health can be implemented.
In outlining and describing goals of occupational health nursing, Morris states that they are inter-linked to the prevention of illness, promoting health, and optimizing the employee’s state of health; this requires the nurse as a profession to constantly update knowledge and technical proficiency in the job to maintain a high-quality standard of patient care (Morris, n.d). And to accomplish quality patient care, the occupational health nurse assumes several different roles that include: providing physical patient care; continual assessment and monitoring of the workplace and employee to identify condition changes and hence take appropriate action; teaching necessary information regarding work hazards, health and safety procedures and the lifestyle factors that affect the health condition of the worker; serve as a patient advocate and liaison between the employee, safety, management, and labor; referral to appropriate community service and lastly, the nurse provide emotional support for employee and the family (Morris, n.d).
In starting the nursing process, the nurse, together with the employee participates in developing interventions that focus on maintaining and improving the employee’s health state. Here, the nurse first identifies those components that make up the individual employee, and the components must be considered in wholesome. Such components include intellectual, which involves the level of information, the ability to learn, perception, sense of control, and participation in personal health maintenance; psychosocial component, which constitutes love, care, belonging, sharing, and necessary support systems; the spiritual component, which include beliefs and attitudes; the physical component, that largely involves lifestyle, work and health history and the current health status (Morris, n.d). To this end, occupational health nursing can be seen to involve efforts of expanding the role of traditional nursing by developing a model that depicts the role of the nurse and how the nurse relates to the health team within the physical and social environment and therefore, the role of the nurse is seen to consist four parts that include team member, manager, professional and patient care provider.
Nurses’ Safety
The safety of nurses has become a hot issue in recent times. The nurses have been commended for performing excellently in their duties in enhancing the quality of nursing care. But to ensure these exemplary services are maintained, mechanisms to ensure the safety of nurses have to be put in place and the nurses on a larger scale are required to take care of themselves. Major areas have been identified by Dr. Bonnie Rogers which pose great health and safety concerns for the nurses, and they include biological and infectious risks, chemical risks, environmental and mechanical risks, physical risks, and lastly psychosocial risks (Rogers, 1997 cited in; Foley, 2004).
Throughout the world, occupational health nurses are convinced that their work has to be accompanied by some risks; and with this realization, various interventions have been made to try and mitigate the risks to manageable levels. For example, three practitioners Castillo, Pizatella, and Stout, in the year 2000, developed a framework that assessed “risks and identifies the most appropriate intervention strategy in risk-provoking situations” (Foley, 2004). They named these interventional approaches as ‘Hierarchy of Controls’. The hierarchy of control offers effective and less effective control interventions in dealing with risks, for instance, “elimination controls/substitution controls, engineering controls, administrative controls, work practice controls, and personal protective equipment controls” (Foley, 2004).
Integrating occupational health nursing model
Rogers states that goal of occupational health nursing is to improve, protect, maintain and restore the health of the workforce within a legal and ethical framework. At the same time, occupational health nursing practice is influenced by conditions in the work setting which may include; resources, corporate culture, work hazards, and workforce characteristics; and these, in turn, operate within a framework of economic, population, and health trends, legislation and politics and technology. Therefore, to address the various risks that compound nurses, the model’s components of assessment, planning, implementation, planning and an additional one of professional development can be utilized.
In assessing the workplace, the nurse needs to collect adequate information about the risks that are presented by chemicals at the workplace such as; sterilizing agents, chemotherapeutic agents, disinfectants and cold sterilants, and ethylene oxide. It will also be important to collect information about the existing hazard control measures in the workplace, emergency potential, and preparedness; moreover, communication and information distribution networks in the workplace will be necessary. After this, the nurse should go ahead in interpreting the data to ascertain the actual and potential health risks posed in the workplace and thereafter recommend the appropriate actions and measures.
The collected data in the assessment phase becomes critical in the next phase of planning where priorities and interventions by the nurse together with the administration should be carried out. A nurse plan will be formulated that should set goals of addressing the identified risks, available resources to effect changes, and if possible, a program of actions to be undertaken in addressing the risks.
The third phase is implementing the plan prepared. At this level, the nurse, together with the workplace administration should bring up a comprehensive and current record of interventions, initiate programs to increase awareness about the risks, and promote positive health and safety practices in the workforce to ensure the safety of the nurses. At the same time, the nurse should continuously participate in the evaluation of environmental data to be making positive adjustments to the program in place.
The next phase will involve evaluation to ensure that the objectives set are being realized. Here, incidence records of injuries in the workplace can be measured to see if they have been reduced. The last stage involves embracing professional development where adequate education and skills will be vital in identifying the potential risks. This is in addition to clarifying how to address the risks, which appropriate measures are safe and how to improve the profession in perspectives of growing risks and hazards in the workplace.
The Death of Terri Schiavo: An Epilogue
On 31 March 2005, American society was to descend on one of the fiercest debates as a result of the death of Terri Schiavo, who to an extent, was disabled and was operating on life-saving machines. However, the death came after a doctor concluded that she was suffering from a cognitive impairment condition which had been analyzed to be a neurological impairment whose chance of survival was minimal; and in the perspective and words of the doctor, the vegetative state could be solved by appropriating death to the girl (Eisenberg, n.d). The death brought up the legal, moral, and professional issues at crossroads with the various professional and interested individuals sustaining intellectual debates and arguments to favor their positions (Eisenberg, n.d). The debate can be seen to have the greatest impact on the nursing professional especially after the nurses were instructed to remove the life-saving machines from Terri and ended up operating without the machines for 13 days, which means no food and water.
Rogers, in developing occupational health nursing, postulated that the goals of nursing could be seen as those to improve, protect, maintain and restore the health of the workforce within a legal and ethical framework. Furthermore, it is the context of practice-the-workforce within a legal or ethical framework that separates the goal of occupational health nurses from other nurses. Rogers further suggested that occupational health nurse practice was influenced by various interrelated factors and the factors operating within a framework of economic, population, and health trends, legislation and politics, and technology. According to the model by Rogers, the occupational nurses have a role of fostering accountability and adhering to ethical issues of the profession. In working within the ethics of the profession, the nurses have the responsibility of operating within the relevant American legislations, always putting the interest of the agency at the forefront while maintaining the integrity of the nursing standards, always to put the needs of the client as a priority, always work to enhance saving of client life and to maintain the client or patient information in highest secrecy.
Terri’s case, to an extent, exposed some of the loopholes as far as ethical conduct of nurses and medical professions are concerned. Indeed, information about Terri’s vegetative state and her being in a position almost of a dead person, the pulling of life-saving machines and feeding equipment which resulted in her experiencing starvation and dehydration, and the eventual medical and philosophical debate surrounding her cognitive impairment and death can be adequately answered using the occupational health nursing model where the nurse has the opportunity to recognize how to deal with such cases and dilemmas that they confront in their workplace each day; for example through assessment, evaluation and adherence to accountability and ethics of the profession.
References
Eisenberg, D. (N.d). The Death of Terri Schiavo: An Epilogue.
Foley, M. (2004). Caring for Those Who Care: A Tribute to Nurses and Their Safety. Online Journal of Issues in Nursing, Vol. 9, No. 3. Web.
Johnson, M. (N.d). Four Basic Metaparadigm Concepts in Nursing.
Morris, L. I. (N.d). A conceptual Model for Occupational Health Nursing Practice. (Attached notes).
Oakley, K. (2008). Occupational Health Nursing. NJ, John Wiley, and Sons.
Songkham, W. et al. (2006). Occupational Health and Safety Programs for Health Care Workers: An application of an Occupational Health Nursing Model. Occupational Health Nurses Society, Vol. 82, No. 4. Thailand, Chiang Mai University.