Executive Summary
The topic of the project is the current state of rates of hospital-acquired pressure ulcers (HAPUs) in US healthcare organizations. The problem of the project is the alarming prevalence rates of HAPUs in Kings County Hospital Center in comparison with the benchmark set by the New York State Department of Health. Kings County Hospital Center has a 3.3 PU rate during October 2014 – October 2015, as compared to the state benchmark of 1.32 (New York State Department of Health, 2016).
The purpose of the project is to get a clear understanding of the differences in the HAPU rates between Kings County Hospital Center and the New York State average. The project focuses on studying the nature and the extent of these differences by performing the data review of the two databases. Since pressure injuries place an enormous physical and economic burden on patients who suffer from permanent pain and are a critical patient safety indicator, it is important to study the identified project problem to help the organization make a difference for patients and their families attempting to address this issue.
Raw data collected from the databases have been used to make conclusions regarding the occurrence of pressure injuries in Kings County Hospital Center in the form of appropriate visualizations. Key performance indicators that have been assessed include the prevalence and incidence rates of PUs, as well as the length of stay associated with this condition for the chosen organization and the NY State. These KPIs align with the hospital’s strategic need of delivering high-quality care to its customers. Based on the obtained results, it has been concluded that prevalence and incidence rates of HAPUs and length of hospital stay for Kings County Hospital Center are greater than the state average indicators.
By examining the extent of these differences, the project adds value to the organization, outlining the ongoing challenges which it faces and giving some recommendations that can enhance business operations, finance, customer service, and organizational learning and growth areas. However, the project’s alignment with the organizational needs could be strengthened by relying on the relevant information about the hospital’s current strategic goals.
Abstract
The project aimed to critically assess the HAPU rates in Kings County Hospital Center based on the NY State benchmark. The organization’s and NY databases were chosen for data collection. Such key performance indicators as the prevalence and incidence rates of stage 2, 3, and 4 pressure injuries and the length of stay of patients with stages 3 and 4 of HAPUs have been considered.
Outcome measures that were used to assess the current status of the problem of HAPUs in Kings County Hospital Center were calculated as the differences between the key performance indicators for the chosen organization and the NY State. Based on the obtained findings, recommendations that could enhance the organization’s performance in business operations, finance, customer service, and organizational learning have been given. Some current evidence-based methods that could be embedded into routine practice by healthcare professionals have been discussed.
Data Review Project Report
The prevalence rates of HAPUs are examined because prevention of this condition is viewed as the critical patient safety indicator and a top priority of the majority of US healthcare organizations (Clark et al., 2014). The project focuses on the examination of the rates of HAPUs in Kings County Hospital Center and assessment of the data by measuring the incidence and prevalence rates of pressure injuries and the length of hospital stay. The paper has been structured to present all the necessary components in a logical fashion. Firstly, the review of the literature with the identification of authoritative sources will justify the purpose and focus of the data review.
Then, performance data will be analyzed, and visual data displays will be developed. Evidence-based recommendations for the future performance of the organization will be given with the consideration of various factors. Finally, a short conclusion summarizing the work done will be made. It is important to study this condition because it contributes to such adverse health outcomes as the deterioration in the quality of life, physical discomfort, increased level of stress, and even death due to serious infections (Wilborn, 2015).
Literature Review
Poor quality of care and a lack of nursing staff make the incidence and prevalence rates of HAPUs grow. Approximately 6.5% of patients die annually due to infections developed as a result of this condition (Roberts et al., 2016, p. 65). According to the quantitative research study, the incidence rate of pressure injuries currently stands at 30% per thousand discharges (Pickham et al., 2018, p. 13). Another quantitative research study found that such an alarming percentage may be explained by the utilization of protocols that are not guided by the best evidence-based practices and high costs of adoption of appropriate technological equipment (Kwong, Lee, & Yeung, 2016).
This conclusion was developed by other researchers who highlighted that support surfaces could prevent the development of PUs (Mcinnes et al., 2015). Research conducted by Ranzani, Simpson, Japiassú, and Noritomi (2016) showed that critically ill patients are particularly at risk as the prediction of PUs using the common tools has not been adequately validated for such patients.
When examining the literature on the current strategies used for HAPU prevention, Wilborn (2015) mentioned that patients who develop pressure injuries in the hospital setting are linked with higher mortality rates and longer length of stay. The authors of a network meta-analysis found that more than 60,000 patients die annually due to complications of the condition (Shi, Dumville, & Cullum, 2018, p. 2). These statistics highlight the need for a critical assessment of the performance of a single hospital-based on the set benchmark in order to evaluate how effectively it tackles the chosen practice problem.
It is worth mentioning that pressure injuries are associated with serious economic concerns. It was highlighted in the study with a cost-utility analysis that HAPUs cost the US healthcare system an estimated $9-11 billion annually (Padula et al., 2018, p. 133). At the same time, the cost of PU prevention per patient is equal to $50 on average (Demarré et al., 2015, p. 1754). However, as was found by the authors of the qualitative descriptive research, apart from costs related to treatment, HAPUs may also result in litigation (Roberts et al., 2017). Considering the discontinuation of reimbursement for HAPUs, enormous stress is placed on hospitals to prevent the incidence of this costly condition, not to mention daunting financial implications for patients.
Data Review
Focus and Situational Analysis
The project focuses on the assessment of the practice problem of HAPUs within Kings County Hospital Center. The chosen key performance indicators for Kings County Hospital Center have been compared to the benchmark set by the New York State Department of Health. It has been found that prevalence and incidence rates of HAPUs for the hospital are alarming (New York State Department of Health, 2016). The project context is defined by its operating environment, which is the review of two databases.
The given report adds value to the organization by evaluating the extent of the selected practice problem and giving recommendations for patient care enhancement. Since the hospital’s mission is to deliver high-quality care to its customers, and its vision is to be the hospital of choice for them, the project is assumed to be important to the organization by helping it serve its patients better. Also, it should be mentioned that the implementation of the interventions suggested in this project may reduce the incidence rates of HAPUs and, as a result, minimize treatment-related costs associated with this condition.
Rationale and Data Description
It is important to get a clear understanding of the organization’s performance related to the practice problem of PUs and compare it to the state benchmark. Results of such a comparison will provide insights into the areas on which Kings County Hospital Center should focus to improve the quality of care delivered to its customers. The framework used to examine the type of data under investigation is the balanced scorecard (see Appendix A). Data that have been measured are the prevalence and incidence rates of stage 2, 3, and 4 PUs and the length of stay of patients with stage 3 and 4 PUs.
The prevalence rate has been measured as the observed number of pressure ulcers per 1,000 patients. The incidence rate has been measured as the number of newly developed PUs per 1,000 patients. The length of stay has been measured as the sum of inpatient days. Based on these key performance indicators, the project outcomes will depend on 1) the difference between the average PU rate for New York and the hospital’s PU rate and 2) the difference between the state average length of stay associated with HAPUs and the average length of stay for the selected hospital.
Data Display
Figure 1 compares prevalence rates of PUs for the selected organization, NY State average, and US average for 2014-2015. It can be seen that while the prevalence rate for the organization is almost the same as the US average, it is more than one and a half times greater than the state average. Figure 2 differentiates the prevalence rate of PUs by the stage of the condition. For each PU stage, the prevalence rate for Kings County Hospital Center is higher than the state average, which means that the trend is consistent. The highest prevalence rates of PUs are observed for the third stage of PUs.
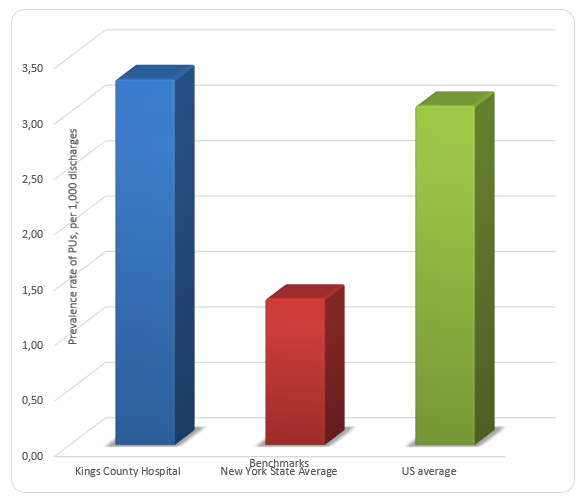
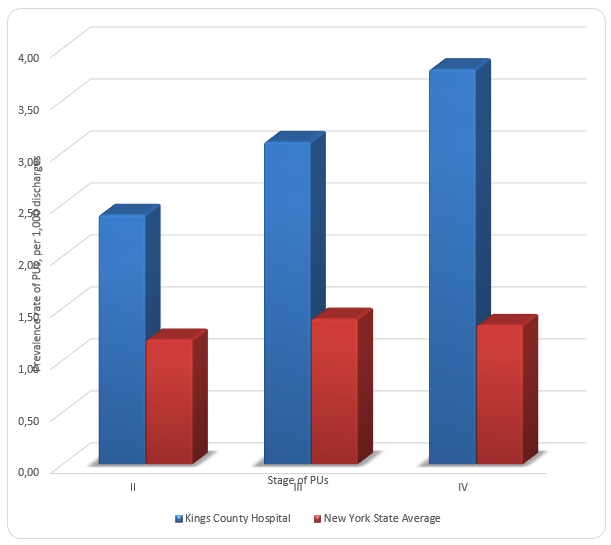
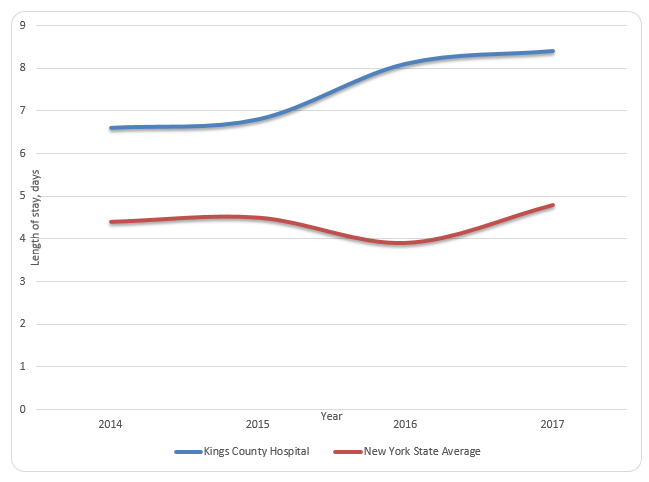
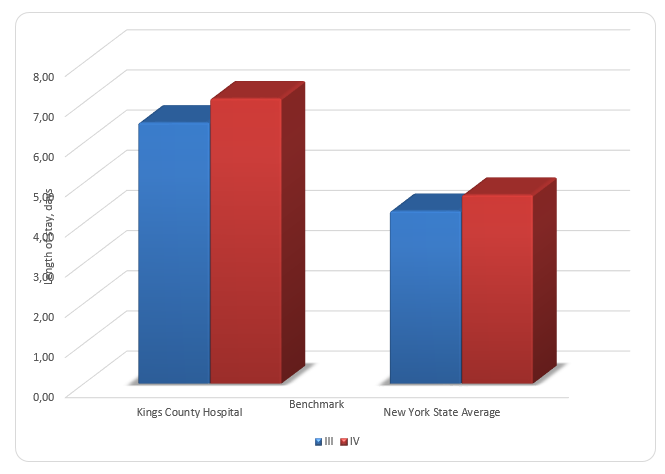
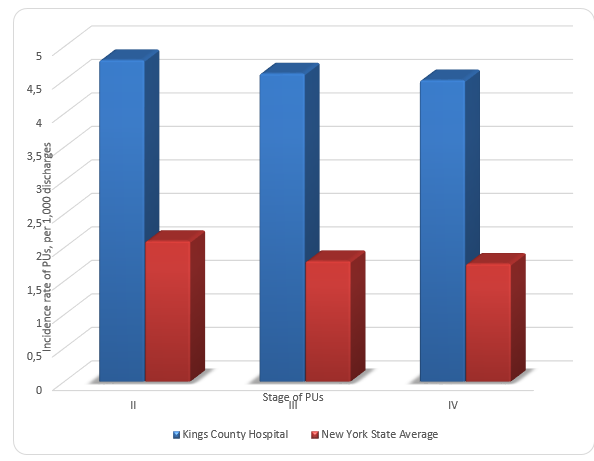
Figure 3 compares the length of stay for patients with HAPUs for the selected organization and the NY State average. It can be seen that, on average, the length of stay for Kings County Hospital Center exceeds the state average by three days. Figure 4 shows that patients of Kings County Hospital Center with both the third and the fourth stage HAPUs have an increased length of stay. Figure 5 compares the incidence rates of HAPUs for Kings County Hospital Center to the NY State average. Incidence rates of stage 2, 3, and 4 PUs are approximately two times higher for the selected organization.
Data Analysis
Kings County Hospital Center significantly underperforms its benchmark for all the key performance indicators outlined in the first part of this report. For the years 2014-2015, the prevalence rate of PUs for the organization is greater than the state average by 2.0. The differences in the prevalence rates by stage 2, 3, and 4 PUs are 1.2, 1.7, and 2.46 correspondingly. The differences in the incidence rates by stage 2, 3, and 4 PUs are 2.7, 2.8, and 2.74, respectively. The differences in the length of stay for patients with 3 and 4 stage PUs are 2.2 and 2.4, respectively. These numbers speak of the extreme severity of the practice problem of HAPUs, which Kings County Hospital Center has faced since 2014. The highest prevalence rates are for stage 4 PUs, and the highest incidence rates are for stage 2 PUs.
However, there are some limitations to the data review findings as they do not reflect the current situation in the hospital. The project can be improved by integrating the data on the key performance indicators for the last three years. Overall, the data is reliable and valid as it has been collected from the databases located on the New York State Department of Health website.
Recommendations for the Future
Considering the alarmingly high key performance indicators associated with HAPUs for Kings County Hospital Center, there is an urgent need to integrate current best evidence-based practices to improve the situation. The first intervention suggested is the introduction of prophylactic dressings as a part of the HAPU prevention strategy. It has been found that the use of prophylactic dressing is associated with a reduction in the incidence rates of HAPUs (Clark et al., 2014). Thus, Kings County Hospital Center could consider the utilization of soft silicone multilayered foam dressings for its patients in acute care units, who are predisposed to PUs.
The second intervention is the use of pressure-relieving support surfaces, such as foam alternatives to standard hospital mattresses. It has been shown that foam mattresses prevent the occurrence of HAPUs, as compared to standard hospital surfaces (Mcinnes et al., 2015). A legal and regulatory factor that is related to the discussed problem is the discontinuation of the reimbursement for HAPUs, and the organizational factor is a lack of pressure ulcer prevention care bundles that are guided by the best evidence-based practices. A possible patient safety factor related to the problem is the low medical staff’s compliance with patient-turning procedures.
Conclusion
In summary, the data review has shown that Kings County Hospital Center has a high prevalence and incidence rates of HAPUs, and, as a result, patients with this condition have an increased length of hospital stay, as compared to the state benchmark. The trend in these key performance indicators has remained steady for 2014-2015. It has been concluded that the organization needs to focus on the improvement of its key performance indicators, considering the physical and emotional burden placed on patients with this condition, as well as the economic ramifications of PUs. Two realistic evidence-based recommendations that are within the organization’s capability have been given. It is assumed that the introduction of prophylactic dressings and alternative support surfaces will reduce the incidence rates of HAPUs.
Leadership insights that have been gleaned from this project relate to the importance of developing a strong professional network and the need for a leader to provide clarity on how a project will add value to the organization. The given report contributed to the organization as it clearly showed the current situation of the practice problem of HAPUs and compared it to the state benchmark, as well as gave useful recommendations for improving the hospital’s performance. The recommendations and the project itself align with the organization’s mission and vision as they are aimed at enhancing the quality of patient care.
References
Clark, M., Black, J., Alves, P., Brindle, C., Call, E., Dealey, C., & Santamaria, N. (2014). A systematic review of the use of prophylactic dressings in the prevention of pressure ulcers. International Wound Journal, 11(5), 460-471.
Demarré, L., Lancker, A. V., Hecke, A. V., Verhaeghe, S., Grypdonck, M., Lemey, J., … Beeckman, D. (2015). The cost of prevention and treatment of pressure ulcers: A systematic review. International Journal of Nursing Studies, 52(11), 1754–1774.
Kwong, E. W., Lee, P. H., & Yeung, K. (2016). Study protocol of a cluster randomized controlled trial evaluating the efficacy of a comprehensive pressure ulcer prevention programme for private for-profit nursing homes. BMC Geriatrics, 16(1), 20-27.
Mcinnes, E., Jammali-Blasi, A., Bell-Syer, S. E., Dumville, J. C., Middleton, V., & Cullum, N. (2015). Support surfaces for pressure ulcer prevention. Cochrane Database of Systematic Reviews, 3(9), 1735–1740.
New York State Department of Health. (2016). Pressure ulcer. Web.
Padula, W. V., Pronovost, P. J., Makic, M. B. F., Wald, H. L., Moran, D., Mishra, M. K., & Meltzer, D. O. (2018). Value of hospital resources for effective pressure injury prevention: A cost-effectiveness analysis. BMJ Quality & Safety, 28(2), 132–141.
Pickham, D., Berte, N., Pihulic, M., Valdez, A., Mayer, B., & Desai, M. (2018). Effect of a wearable patient sensor on care delivery for preventing pressure injuries in acutely ill adults: A pragmatic randomized clinical trial (LS-HAPI study). International Journal of Nursing Studies, 80, 12-19.
Ranzani, O. T., Simpson, E. S., Japiassú, A. M., & Noritomi, D. T. (2016). The challenge of predicting pressure ulcers in critically ill patients: A multicenter cohort study. Annals of the American Thoracic Society, 13(10), 1775-1783.
Roberts, S., Mcinnes, E., Wallis, M., Bucknall, T., Banks, M., & Chaboyer, W. (2016). Nurses’ perceptions of a pressure ulcer prevention care bundle: A qualitative descriptive study. BMC Nursing, 15(1), 64-74.
Roberts, S., Wallis, M., Mcinnes, E., Bucknall, T., Banks, M., Ball, L., & Chaboyer, W. (2017). Patients’ perceptions of a pressure ulcer prevention care bundle in hospital: A qualitative descriptive study to guide evidence-based practice. Worldviews on Evidence-Based Nursing, 14(5), 385-393.
Shi, C., Dumville, J. C., & Cullum, N. (2018). Support surfaces for pressure ulcer prevention: A network meta-analysis. PLOS One, 13(2), 1-29.
Wilborn, W. (2015). Pressure ulcer prevention strategies. Nursing Made Incredibly Easy, 13(6), 10–12.