Introduction
Gibbs’s reflective cycle is an important element of nursing practice, as it allows them to improve their practice, find strong and weak sides, and fix them. Therefore, I will use it to reflect on my practice, describe and evaluate it, to understand how I can improve it. Lack of knowledge, uncertainty, and negative experiences may be resolved by doing this, as I will be able to see what I should learn and how I should act to experience fewer negative feelings (Mlinar Reljić, Pajnkihar, and Fekonja, 2019).
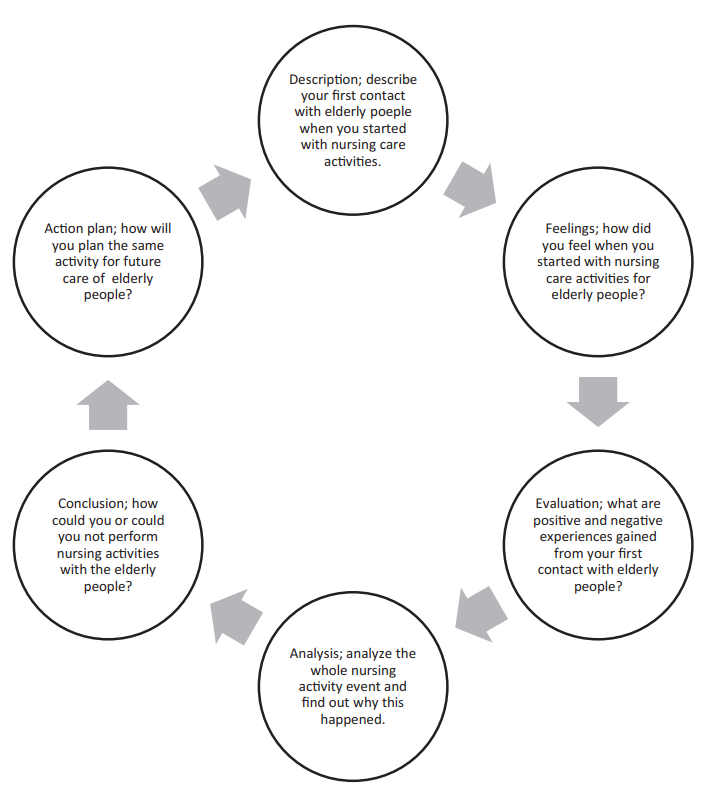
One can see the cycle in Figure 1: each stage contains a question or task, answering which one can improve one’s competency and experience. There are other reflection models, such as Kolb’s Experiential Learning Cycle, which has four elements: experience, observation, conceptualization, and action (University of Cambridge, 2021). However, I have used a Gibbs model, as it is the most detailed, which enables much more concise, thorough, and efficient reflections than by using other, less detailed models.
In my first placement, I encountered various experiences, but the two most prominent ones were the cases with Andrew, my patient, and Mary, my colleague. I had changed their names, as I should not breach the confidentiality of those with whom I work, according to the NMC Code (Nursing and Midwifery Council, 2018). Andrew was a patient with depression, who fell into an aggressive conflict with another patient, and I was able to calm him down by showing him that he was not abandoned and administering medication. Mary loves to teach everyone in her own manner, while I really do not like when someone tries to impose their point of view on me. It caused negative feelings in both of us, and there was a case when I was so irritated that we became engaged in a conflict.
Description
In my first placement, I encountered positive and negative experiences. The most positive factor was the possibility of learning something new, and I was very curious about medication. I worked with people with mental issues, and my task was observing them, talking with them, and administering medication. The first several days were more nervous, but I adapted quickly, and all the next days, up to today, were mostly calm and happy. I feel confident when working with patients, knowing that I only need enough knowledge to reach my goal of helping people.
Working with one of my patients, Andrew, became a challenge for me, which I think I passed successfully. He came at approximately 3:00 PM with depression symptoms and quickly became distressed as there were other patients who approached him without any respect. One of them, with whom I did not expect to work, started to shout at Andrew, and he began to shout in response, saying various offenses to his opponent. I approached Andrew after 5 minutes of their aggressive conflict, asked him to listen to me, and proposed to him to communicate about his problem and aggression, and he agreed immediately.
For approximately 15 minutes, he spoke of his personal issues and constant depressive episodes, which prevented him from working and living happily. It causes aggression, and he thinks that no one wants to understand it, only blaming him for his shouts. When I listened to him carefully and advised him to take several medications to reduce symptoms, he was very thankful and happy that there was someone who cared; his aggression went away after that.
Working in teams was much harder for me than working with a patient alone. While I can certainly know what to do with a patient, things are not always clear with colleagues. When they are kind and open, it may be interesting to speak with them, and I enjoyed this experience. Unfortunately, there are some whose characters are drastically different from my own, and I strive to cope with negative feelings and mediate the conflict with them.
There was Mary, my colleague with whom I had an uncomfortable experience: she was quite dominant and enjoyed teaching others in her quite commanding way. I had only several talks with her, but it was enough to spoil my mood for the whole day. Mary positioned herself as generous, kind, and ready to share her knowledge. However, she tried to notice all my mistakes in work and personal weaknesses and then lectured me about what was wrong with me. When I disagreed, she started to insist, talking that I could be more active at work; I was dissatisfied by this, and we argued. It happened in the evening, at 7:20 PM, and resulted in our unwillingness to work together at all, creating considerable tension in the whole work collective. While we continue to see each other and work together, we avoid communicating, speaking only shortly on work themes.
Feelings
My feelings were different during this placement, both positive and negative ones: the most frequent were stress and curiosity. While it was hard to deal with mentally ill patients, as they are unpredictable, it was more interesting than scary for me to watch for them and communicate with them. Patients were usually desperate and needed care and understanding: they wanted to see that there was someone who was not indifferent to them (Arnold and Boggs, 2017). As I am an empathetic person, while not being very sensitive, I was able to fulfill their expectations and help them.
One of the most negative feelings I experienced was social awkwardness due to the uncertainty of how I should behave with my colleagues, which resulted in my closedness. I tried to remain professional with colleagues, maintaining kind treatment, but it was hard when our characters were drastically different (McKibben, 2017). Mary was the most prominent case: I felt no curiosity or interest but sheer irritation when she tried to teach me what I should do. She did it dominantly, showing that I knew less and must do as she said, which caused my negative reaction.
I was happy to apply my knowledge about various medications in practice and see how clinical symptoms look in real life. The Andrew case has shown me that I do not mirror other people’s negative feelings, and thus, I feel confident about my ability to help ill people recover. The main challenge for my future practice is the necessity to work on my communication and emotional intelligence skills (Isobel and Delgado, 2018). As the Mary case shows, my emotional intelligence is quite low, and thus conflicts lead to my negative emotions that hinder my performance, relationships, and life quality (Szczygiel and Mikolajczak, 2018). I need to work on my communication and conflict-solving skills to ensure that my professional relationships will be efficient.
Evaluation
I realized that while I can work with patients well, I was not ready to work in a collective. I don’t mirror other people’s negative emotions, but I explode easily when someone openly confronts me, even with positive intentions.
Therefore, I need to work on my perception of myself and others to ensure that the situation with Mary will not repeat (Lee and Doran, 2017). Mary just wanted to show me her opinion on how to make things done and wanted to hear my feedback, so next time, I should not confront my colleagues but listen to them (Isobel and Delgado, 2018). Emotional intelligence is crucial for managing my emotions: it means the ability to see the situation from various perspectives and proceed with my emotions easily, so I need to work to increase it (Szczygiel and Mikolajczak, 2018). Therefore, I am generally satisfied with my experience, but I need to pay more attention to communication, teamwork, and the management of my emotions.
Analysis
Confidence, which can also be called moral courage, is one of the most important qualities of the nurse, and as evaluation shows, I should train it further. According to Bickhoff, Sinclair, and Levett-Jones, (2017), moral courage is the nurse’s ability to act in the best possible way and be ready to bring all responsibility. Emotional intelligence is crucial for developing it, and I should learn to see the situation from other people’s perspectives and their feelings (Szczygiel and Mikolajczak, 2018). I love this idea and try to reach it in my practice, as I believe that the nurse should help people, and this was my primary motivation to work in this field.
While I was ready for problems with patients and was ready to deal with them, I was not prepared for issues with my colleagues. Communication skills are essential, as good interpersonal relations are necessary for working together and experiencing exchange (Lee and Doran, 2017). My conflicts with Mary led to the situation when I could not fully rely on her, and she, similarly, could not rely on me, which is highly undesirable at work (Arnold and Boggs, 2017).
If I feel offended, I should not confront others but write about my perspective and report to other colleagues and management staff, letting them help us solve the conflict (Najafi et al., 2017). In addition, I should listen to my colleague and be ready to apologize first, showing that I am professional enough to solve work conflicts safely (McKibben, 2017). I am sure that this would solve the situation with Mary, so I will work to improve my emotional intelligence, conflict analysis, and solving techniques, and the ability to perceive others without confrontation.
Conclusion
I elucidated several vital consequences from the analysis and evaluation of my experience. First, I should improve my knowledge of medications and understanding of patients, as it is my strong side, and I really love it. It will not only make me closer to the ideal of moral courage but strengthen my position at work, as other nurses will trust me more (Bickhoff, Sinclair, and Levett-Jones, 2017). In the case of Andrew, my successfully calming him down inspired me, and I have learned how I can do my work efficiently. I am ready to work with other patients and help them to calm down and recover.
Second, I need to learn how to meditate and stop conflicts, even if I have tight relationships with the person I am communicating with, and resolve my negative emotions. Bad feelings may result from a simple misunderstanding, as it was in my case with Mary. I need to distinguish true workspace violence from a simple misunderstanding. When I am offended, it is better to resolve the conflict when no direct violence is present (McKibben, 2017).
To do that, I can first restore my emotional state, change my attitude, and then start to talk with another party immediately or after some time. Otherwise, I can report to the management team, raising the concern and describing to them which damage I received and from whom (Najafi et al., 2017). I should become more emotionally resilient, being able to perceive others’ emotions and express my own more freely and less destructively (Delgado et al., 2017). All people are different, and it is crucial to improve my emotional intelligence, learning to perceive situations from various perspectives and not respond with negative feelings.
Third, communication is much more important than I thought: I learned how a lack of communication might cause problems, and, reflecting on them, I figured out how they can be solved. I need to improve my communication skills, as they are crucial in nursing work: listening, understanding others, evaluating their words, and clearly formulating my answers or suggestions (Arnold and Boggs, 2017). If we are in conflict, as in the case of Mary and me, we cannot work together efficiently. According to Lee and Doran (2017), good practice is a constant evaluation of the connection with understanding what was wrong. It would be good to try this practice with Mary, and I will do this as soon as possible. In addition, it would be a good and professional sign to apologize first.
Action Plan
During my further placements, I will be more careful with other nurses with me and will try to choose to team with those who are kinder and more suitable for me. For this placement, I totally ignored this, being focused only on patients and medications. I plan to improve my emotional intelligence and resilience skills by learning how to perceive situations from various perspectives and express negative emotions in a non-destructive way (Szczygiel and Mikolajczak, 2018).
For example, when I have anger, I can try to relax and imagine how my opponent feels immediately after this. I would change my attitude quickly, and instead of aggression, I would feel a strong desire to resolve the conflict, and my opponent will likely support me in that. In addition, it will increase my empathy and enable me not only to help my patient recover but be more supportive, warm, and understanding of them.
I will also work on my communication skills, especially those connected with nurse-patient communication, teamwork, and establishing good working relationships. I will try to reconcile with Mary, admitting I was wrong by arguing with her, apologizing, and asking her not to teach me this way (Arnold and Boggs, 2017). In the future, in case of conflicts, I will do my best to remain calm and, after that, will try to reassure my opponent that they are safe and will be listened to and understood (McKibben, 2017). If they continue, I will go away and will try to speak with them after some time. It should be not long after the situation, typically within the next 30 minutes, and I should be ready for possible misunderstandings. If they arose, I would offer my colleague to discuss them with me to avoid offending their interests (Isobel and Delgado, 2018). It will probably solve our conflict with Mary and, possibly, keep our professional relationships good.
Reference List
Arnold, E. and Boggs, K.U. (2017). Interpersonal relationships: Professional communication skills for nurses. 7th ed. St. Louis, Missouri: Elsevier.
Bickhoff, L., Sinclair, P.M. and Levett-Jones, T. (2017). ‘Moral courage in undergraduate nursing students: A literature review’. Collegian, 24(1), pp.71–83. Web.
Delgado, C., Upton, D., Ranse, K., Furness, T. and Foster, K. (2017). ‘Nurses’ resilience and the emotional labor of nursing work: An integrative review of empirical literature’, International Journal of Nursing Studies, 70(70), pp.71–88. Web.
Isobel, S. and Delgado, C. (2018). ‘Safe and collaborative communication skills: A step towards mental health nurses implementing trauma informed care’, Archives of Psychiatric Nursing, 32(2), pp.291–296. Web.
Lee, C.T.-S. and Doran, D.M. (2017). ‘The role of interpersonal relations in healthcare team communication and patient safety’, Canadian Journal of Nursing Research, 49(2), pp.75–93. Web.
McKibben, L. (2017). ‘Conflict management: Importance and implications’, British Journal of Nursing, 26(2), pp.100–103. Web.
Mlinar Reljić, N., Pajnkihar, M. and Fekonja, Z. (2019). ‘Self-reflection during first clinical practice: The experiences of nursing students’, Nurse Education Today, 72(72), pp.61–66. Web.
Najafi, F., Fallahi-Khoshknab, M., Ahmadi, F., Dalvandi, A. and Rahgozar, M. (2017). ‘Antecedents and consequences of workplace violence against nurses: A qualitative study’, Journal of Clinical Nursing, 27(1-2), pp.e116–e128. Web.
Nursing and Midwifery Council (2018). The Code: Professional standards of practice and behavior for nurses, midwives and nursing associates. NMC. Web.
Szczygiel, D.D. and Mikolajczak, M. (2018). ‘Emotional intelligence buffers the effects of negative emotions on job burnout in nursing’, Frontiers in Psychology, 9. Web.
University of Cambridge (2021). Reflective practice toolkit: Models of reflection. Web.