Introduction
Climate change refers to the long term alteration in the statistical properties of the weather patterns within a specific region, or even globally. Some of these changes would include temperatures, precipitation, and cloud cover, among others. Contributed factors to climatic change are classified into two main categories; natural and human-induced factors. Various studies have shown that human activities on the land and the atmosphere have contributed greatly to change in climate, among other factors. A good example of the common human activities said to have contributed to changes in weather patterns would include things such as the burning of fossil fuels, deforestation, and changes in wetland building or construction. More importantly, these changes in weather patterns, as witnessed in the contemporary world, have also occurred as a result of interactions between the atmosphere and various other geographic, biological, chemical, and geologic factors within the Earth system. Human-induced factors have over the time resulted in high levels of greenhouse gases such as carbon dioxide, methane, nitrous oxide, water vapour, and ozone in the earth’s atmosphere.
These changes in the global climatic conditions have continued to pose many impacts on the lives of global populations. Climate change has been rated among the top issues which have continued to draw much concern and interest in modern study and research. Climate change is a major global issue that has continued to pose countless threats to human safety, health, and survival on various parts of the earth over long historical moments (Hughes 2003).
Some of the major impacts associated with the issue can be felt in the form of increased temperatures on the earth’s surface, rise in sea levels, changes in precipitation, increased intensity of serious weather events, e.g. hurricanes and tornadoes, melting of the permafrost, drop in agricultural yields resulting to longer and severe drought periods, the spread of vector-borne ailments, and acidification of sea waters resulting to destruction of coral reefs and drops in fishing yields. It is obvious from research findings that, the rate of global warming, which stands high as a major effect of the climate change, may not be slowed sufficiently to put a significant control on the foretold climatic changes. A consequence of the issue, however, is that changes to biological and physical systems will continue to pose serious impacts on the global population and the only option there is would be for people to adapt to all these current and potential threats and try avoiding the adverse consequences that are likely to present from them.
Scientists have always expressed their concern that the global change in weather patterns has constantly increased the risk of heatwaves, hot weather, heavy rainfall downfalls, altered drought patterns, and bushfires. However, among the vast implications outlined above, all of which come by as a result of altered global weather patterns, consequent impacts of the issue on human health is far much understood. Climatic fluctuations have seriously continued to affect human health in most regions of the world. More extreme heatwaves as a result of climate change have increased the threat of heat-related human deaths. Respiratory disorders have also been observed to have continued to get to their worse levels, as the quality of air deteriorates.
More importantly, extreme weather patterns and events have also contributed to much greater risks of loss of human life, disease and mental disorders. The risks of health associated with climatic changes are obviously indirect and are likely to be realised through food products, water flows, mosquito and bacteria flows, and the highly-concentrated greenhouse gases in the atmosphere, among other effects (Mctainsh & Lynch 1996). This project provides an analysis of the impacts of climate change on human health in New South Wales (NSW), Australia. This project has offered a concise understanding of current and potential climate impacts as well as associated social implications of global weather fluctuations on human health. Apart from observing the many effects of health presented by the climate change on the Australian population, this project also proposes a number of ways by which people in those specific regions can adapt and mitigate those changes.
The Impacts of Climate Change on Human Health in Sydney, Australia
Changes in average climatic conditions and the increase in the intensity of extreme events as castigated by fluctuating weather patterns do have a significant influence on human health. For instance, an increase in the intensity of extremes of precipitation, temperatures and wind speed has been known to bring serious implications for morbidity and mortality. On top of these impacts of direct heat, the change in climatic conditions is also associated with a range of other indirect impacts on human health and these would include changes in the seasonality of vector-borne ailments, increase in food and water-borne diseases, increase in impacts of air pollution due to ground-level ozone and particles, and shifts of populations, among other associated impacts on general human health. Storms and increased floods are most likely to increase the risk of non-fatal accidents and deaths. Also, mental health effects such as anxiety and depression have also been reported in some regions of the NSW, following extreme events caused by changes in weather patterns.
Moreover, floods are observed to have other health effects, including the risk of vector-borne disease outbreaks and diarrhoea, among other health complications. Change in climate has progressively increased the risk of infectious ailments, particular those diseases which are common in warm areas and are transmitted by mosquitoes and other common insects (Currie & Jacups 2003). Examples of these vector-borne diseases include dengue fever, encephalitis, malaria, and yellow fever. Also, prolonged drought periods have sometimes caused water quality issues and increased concentrations of pollutants. This, coupled with high water temperatures, is likely to encourage algae blooms, which has constantly affected the quality of water in NSW Sydney areas, particularly Sydney. The growth of algal blooms has been more frequent in the region of late than in any other moment in history, and this has constantly facilitated the breakout of serious ailments which tend to accompany algal blooms, such as cholera. All these effects have been observed in some parts of New South Wales, as serious effects of the global climate change.
According to reports from different organizations, about 7.2 million people, almost 32 per cement of the entire Australian population, live in New South Wales. As it would be observed, NSW is among those regions which have been seriously affected by the change in climatic conditions in Australia. Among other areas, the impacts on human health are immense in this region. For instance, it is obvious that more people in NSW are likely to suffer heart-related ailments and even death, as the number of days having more than 35 degrees Celsius, continue to become more frequent. Following the findings of research funded by OEH to determine the impacts of extreme heat on human health in some regions of New South Wales, people having various underlying conditions of health were observed to have been more susceptible to extreme events of heat. New South Wales is rapidly growing hotter and drier, compared to other parts of Australia, with heatwaves have increased in intensity and duration, in the greater Sidney area. Most parts of NSW are observed to have become much drier over the last ten decades, and it is now generally accepted that most of the region will experience a hotter and drier climate with increased extreme events (Connor & Albrecht 2004). This prolonged drying trend, however, has increased the risk of extended droughts. It has been estimated that about 176 people aged 65 years and above die on an annual basis in Sidney from deaths associated with heat, and this is likely to reach a rate of about 417 by the year 2012.
The following figure indicates the no. of days over 35 degrees projected for NSW and the surroundings.
According to a recent study that was conducted to determine emergency hospital admissions in various regions of NSW, there was a relative increase in heat-related cases, on extremely hot days. A research conducted by the Commonwealth Scientific and Industrial Research Organization (CSIRO) on the Sydney region revealed the possibility of hospital admissions increasing to 40 per cent, due to higher levels of ozone in the air, which has been associated with heightening the intensity of hot days in the region (Watson & McMichael 2001).
Additionally, People with existing health conditions such as respiratory diseases and mental disorders were observed to be more susceptible to injury and death related to heat. People from New South Wales are said to be more exposed and susceptible to deaths associated with the cold than the heat. In this regard, the rate of temperature-related deaths is estimated to approach 1,906 by the year 2100 if no mitigation approach is reached, while compared to 2,754 in a region that lacks human-induced effects. Mosquito-borne ailments, such as Murray Valley Encephalitis and Dengue, have sometimes resulted in serious life-threatening diseases and ailments to the NSW population (Pittock 2003). Mosquito-borne diseases and issues have been noted in some region of New South Wales and its surroundings, particularly under moderately warm and wet conditions of climate.
Increased intensity and frequency of extreme climate events such as floods and storms have also had a significant impact on the health of the NSW population. This is evident in cases where food gets spoiled as a result of improper preservation due to the impact of these extreme events, thus leading to illnesses among the people. Other climate change risks of health observable in Australia’s New South Wales region would consist of food-borne infectious diseases, severe weather events such as bushfires, mental-related problems and consequences, and pollution of the atmosphere, among other significant effects.
As it would be expected, adverse impacts of fluctuating climate conditions on human health have been high among specific categories of people, such as those with low-incomes, the elderly and those who are weak from diseases. More importantly, New South Wale’s climate is set to change with time, probably to the worst, and this is likely to steer mortality and morbidity from bacteria gastroenteritis, air pollution, thermal stress, flooding, vector-borne ailments, and bushfires among other serious effects (Russell 1998). It is apparent that the type of potential impacts that are likely to present here would reflect the climatic conditions of the region and that of the whole world. However, the rate by which these potential impacts would be realized in NSW will entirely depend on how the population in the region responds to the climate change challenges facing them.
Literature Review on Climate Change Impacts on Health
Change in climatic conditions and variations continue to impact every segment and resident of New South Wales in Australia. This review tries to identify and analyze some of the available literature which highlights the impacts as well as the potential adaptations relevant to NSW and the surrounding regions. There has been long writing history of the international issues affecting the contemporary world, and the climate change agenda, which has been necessitated by the heightening issue of global warming, has been at the forefront, among these issues. Among other impacts, the effects of climate change on health and the overall wellbeing of humans is now very concrete from evidence which has been cited in an extensive platform of literature.
Most of the featured literature here has been retrieved from publications by the Commonwealth Scientific and Industrial Research Organization (CSIRO) and the NSW Department of Environment Climate Change and Water (DECCW). As it has been revealed from a great deal of all these literature, the world is not the same today, considering the adverse levels of pollution in the air. Today, human health is endangered by climate change, among other environmental changes, and there is no doubt about that. There are adverse climatic influences on infectious diseases in history, among other health issues. However, the causal processes which affect health outcomes are observed to be complex, various posing serious effects on demographic stresses, social conditions, governance, and also the superimposed issues of changes in weather patterns.
Throughout the planet, the prevalence of serious ailments and other threats to health depends entirely on climatic conditions. High constant temperatures have contributed an immensely indirect loss of human life, while issues related to weather fluctuations in ecological systems have continued to impact the occurrence of serious infectious ailments among humans, as it has been witnessed in many parts of New South Wales. Extreme events as a result of changed climatic conditions, particularly wind and rainfall, are not uncommon in most parts of NSW, as they would be influenced by the extra-tropical cyclones in the regions (CSIRO, 2011). It has also been observed that high temperatures tend to increase water and air pollution, which in turn poses great harm to human health. As it would be concluded in the Intergovernmental Panel on Climate Change of the year 1997, global populations are highly exposed to change in climatic conditions through fluctuating weather patterns, which are characterized by frequent and more intense extreme events of weather and notable changes in air, water, economy, ecosystems, and food quantity and quality.
Global changes in climatic conditions have greatly influenced the frequency of extreme events of weather in various parts of NSW. In this regard, tropical cyclones have been observed to go up in most of those regions as sea surface waters continue to warm. Cases of floods have also been reported, due to the intensification of the hydrological cycle. The largest impact, however, has been realized in most parts of Australia where heat waves have been reported to be heightening. The changes in the intensity and frequency of cold spells and heat waves have constantly affected the seasonal patterns of mortality and morbidity in many regions of New South Wales. According to a recent report by CSIRO, changes in climatic conditions over the years has progressively affected human health through a number of indirect pathways such as the yield of food-producing systems at sea and on land, patterns of infectious ailments and disorders, and contribution to the loss of biodiversity. It is also apparent that climate change has also contributed to destabilising and weakening services of the ecosystem upon which the majority of the human society around those regions depend for their survival. The effects are minimal at this stage but are expected to progressively increase in all regions in the near future if effective mitigation and adaptation activities are not implemented.
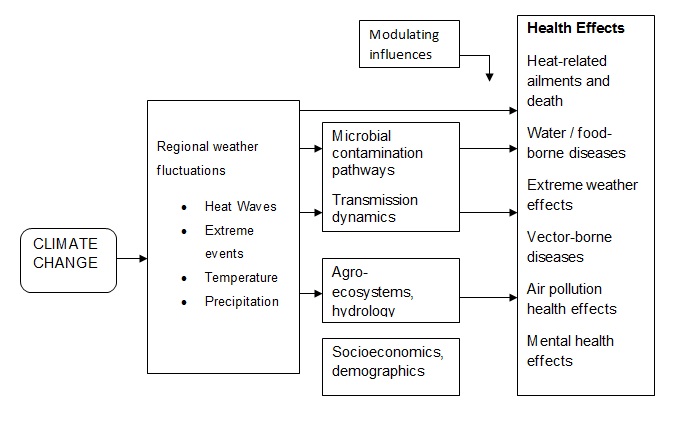
The following figure indicates some of the major pathways by which climate change has affected human health in NSW, Australia.
Data and Methods
Literature review and analysis of available data and information on the issue are the methodologies used in this project. It was easy to identify some of the current and potential impacts of climate change in Sydney, as it would be witnessed from various forms of climatic change effects. This project was carried out in two main phases; phase 1 and phase 2. The initial phase aimed at identifying some of the major potential health impacts that arose from the change in climatic conditions in the identified region and the possible consequences these would possibly bring to the environment. The second phase, however, would focus on assessing the potential health impacts that would arise from fluctuating weather patterns in Sydney and other parts of New South Wales, as a result of changing climatic conditions.
The following table summarizes the potential health impacts as a result of climate change in Australia is relevant to their pathways and other driving factors.
In trying to identify the above climate change impacts on health, it was very important to identify the common various aspects of vulnerability, and this would include economic, regional, infrastructure and social services. The analysis however, highlighted various vulnerabilities that would be common to various potential health impacts.
Economic vulnerability
Economic vulnerability was observed to be very common for many potential health impacts resulting from change in climatic conditions in NSW, particularly within the boundaries of Sydney, where the study was conducted. Regions having a strong link between climate and economic prosperity were considered to be a bit more sensitive to change in climatic condition compared to others. Economic vulnerability however, was directly linked to adaptive capacity. For instance, it would be less likely for the households, individuals or communities with minimal socio-economic levels to be able to afford possible price increases in various goods and services, and important adaptive or mitigation measures. A good example here would include inability to access adaptive or mitigation approaches for heat waves and temperature increases, such as air conditioning and energy efficient housing facilities. Also, people of low income levels are more likely to be more vulnerable to increase in price in various goods and services that would be of basic requirement to their normal lifestyles (Green & Preston 2006). Some of these goods and services would include things such as Food, energy, water, and insurance, among other requirements.
Regional vulnerabilities
Regional vulnerabilities are expected to occur in terms of sensitivity, exposure and the capacity of adaptive. As it would be observed from this study, climatic conditions would be experienced in the various parts of the identified region i.e. Sydney. For example, levels of temperature may not be the same in all parts of the region. This has the meaning that, some parts are likely to experience higher temperatures while others would register lower levels (Braaf 1999). In this study for instance, the communities around or near coastal regions, were identified to be potentially vulnerable to storms, rise of sea levels and surges, among other extreme weather events. However, in terms of adaptive capacity and sensitivity, places having a high proportion of isolated communities would be identified to be more vulnerable to a wide range of potential climate change impacts and effects.
Infrastructure and services vulnerability
Many infrastructures and services in the modern society are designed based on historical climate data. In that case, there is much risk these planning approaches may be inadequate for future climate and weather conditions. It would be possible for vulnerability to present from a combination of increased demand for basic services and diminishing resources or from direct physical destruction to available infrastructure. It is obviously clear that, the health of communities would be entirely dependent on access of reliable services and infrastructure. In this regard, any changes in provision capacity of things such as clean and safe water, communication, medical facilities, reliable energy, and transport, among other basic needs is likely to bear both direct and indirect impacts on human health. This analysis would identify regional and remote communities to be in possession of limited resources in terms of health services. However, potential climate change impacts on coastal infrastructure was noted to be of major concern, as most planning guidelines in the coastal regions around NSW had limited adjustments for projected sea level increases.
Social vulnerability
Different populations groups and sub-groups were observed to be more vulnerable to most of the identified potential impacts resulting from change in climatic conditions in Sydney. These groups particularly consisted of populations whose status of health was at a higher risk. These groups included the elderly, children, the disabled, indigenous groups of people, the homeless, and people with other complicated health issues. However, the vulnerability rate of these groups would vary widely, depending on specific health impacts affecting them and other important factors. Among these groups, indigenous populations were noted to be more vulnerable to most of these impacts compared to non-indigenous groups, due to their lower living standards and existing problems of health. As it would be observed, inability to access basic infrastructure in the regions inhabited by indigenous groups or communities is most likely to result to great vulnerability as a result of poor adaptive ability (McMichael & Hales 2006).
Aged groups and children were also identified to be vulnerable to many potential health impacts, as a result of change in climatic conditions in the region. In this line, impacts from increases in temperatures and heat waves were observed of major concern here. Food and water borne ailments and respiratory effects, resulting from poor air quality were the other impacts observed to be affecting these categories of people. Children, it was observed, would be more sensitive to various health impacts for a number of reasons including higher breathing and metabolic rates and immature immune systems. Moreover, pre-existing diseases and medication are also likely to increase vulnerability of this population group to various potential health impacts.
Specific vulnerabilities
Apart from the various vulnerabilities described above, other potential health impacts would apply to specific vulnerable groups. For instances, people who’d normally spend a lot of their time indoors, either in lifestyle and occupational activities were noted to be vulnerable to heat-related diseases, vector borne ailments, and UV exposure, among other specific health impacts. It was also observed that, people who lived closed to mosquito breeding areas were also a bit more vulnerable to vector borne diseases and ailments compared to those who lived in dry areas, safe from habitats that would encourage mosquito breeding and growth.
Possible Responses and Limitation
After considering the existing coping capacity, it was observed that many areas on New South Wales, particularly Sydney, which is largely featured in this project, are well-positioned to respond and adapt to climate change events as they present. However, as it would be observed, some areas would require extra responses that would help in establishing strong and effective adaptive capacity in dealing with those impacts.
The table below identifies the coping capacity and associated limitations.
Conclusion and Implications
As it is evident from this project, climate change has progressively continued to pose diverse direct and potential health impacts to the Australian population, particularly the regions within North South Wales. The implications of various health impacts, as presented in this project presents a big challenge to relevant organisations and institutions, both public and private, to come up with adequate levels of advance management, planning and concern to reduce climate change impacts on human health.
This project has examined and analysed a number of adaptation measures that have been implemented in various segments of the NSW communities, in an attempt to slow down effects of climate fluctuations on health. Informed strategies have been applied to identify some of the major impacts of climate change on health in Sydney and other regions of NSW. This approach has played a key role in assessing the levels of adaptive capacity needed to ensure that effective adaptation strategies are implemented to address the complex issue of climate change and the chain of direct and indirect impacts this poses on health. This project creates room for further research on the field, to identify new adaptation strategies in addressing the complex issue of climate change. In this regard, there is need for extra funding for research programs on the issue, more health care personnel in indigenous communities and other vulnerable regions, improved treatment infrastructure and basic needs and amenities, among other factors that would contribute positively towards the effort of reduce impacts of climate change on health.
Reference List
Braaf, R 1999, ‘Improving impact assessment methods: climate change and the health of Indigenous Australians’, Global Environmental Change, vol. 9 no. 7, pp. 95-104.
Connor, L. and Albrecht, G 2004, ‘Environmental change and human health in Upper Hunter communities of New South Wales, Australia’, EcoHealth, vol. 1 no. 7, pp. 25-34.
Currie, B. & Jacups, S. 2003, ‘Intensity of Rainfall and Severity of Melioidosis, Australia’, Emerging Infectious Diseases, vol. 9 no. 6, pp. 1538-1542.
Green D & Preston B 2006, Climate Change Impacts on Remote Indigenous Communities in Northern Australia, IDP Education Australia, Sydney.
Hughes, L 2003, ‘Climate change and Australia: trends, projections and impacts’, Austral Ecology, vol.28 no. 4, pp. 423-443.
McMichael, A & Hales, S 2006, ‘Climate change and human health: present and future risks’,The Lancet Mar, vol. 11 no. 367, pp. 859-69.
Mctainsh, G. & Lynch, A 1996, ‘Quantitative estimates of the effect of climate change on duststorm activity in Australia during the Last Glacial Maximum’, Geomorphology, vol. 17 no. 36, pp. 263-271.
Pittock, B 2003, Climate Change: An Australian Guide to the Science and Potential Impacts, Australian Greenhouse Office, Canberra, Australia.
Russell, R 1998, ‘Mosquito-borne arboviruses in Australia: the current scene and implications of climate change for human health’, International Journal for Parasitology, vol. 28 no. 6, pp. 955-969.
Watson, R & McMichael, A. 2001, ‘Global climate change – the latest assessment: does global warming warrant a health warning?’ Global Change and Human Health, vol. 2 no. 14, pp. 64-75.